Contents

This edition first published 2010 © 2010 W. Whyte
First edition 2001 © W. Whyte
Published by: John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, United Kingdom
For details of our global editorial offices and for customer services please see our website at .
The right of the author to be identified as the author of this work has been asserted in accordance with the Copyright, Designs and Patents Act 1988.
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher.
Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their respective owners. The publisher is not associated with any product or vendor mentioned in this book.
This publication is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold on the understanding that the publisher is not engaged in rendering professional services. If professional advice or other expert assistance is required, the services of a competent professional should be sought.
Library of Congress Cataloging-in-Publication Data
Whyte, W.
Cleanroom technology: fundamentals of design, testing and operation/W. Whyte. -- 2nd ed.
p. cm.
Includes index.
ISBN 978-0-470-74806-0 (cloth)
1. Clean rooms. I. Title. TH7694.W48 2010
620.8'6--dc22
2009031436
About the Author
William (Bill) Whyte is an Honorary Research Fellow at Glasgow University. He has been involved with cleanrooms for over 45 years and has the useful dual qualifications of a BSc in microbiology and a DSc in mechanical engineering.
He has published over 130 reports and papers on contamination control and cleanroom design. He wrote the first edition of this book in 2001 and has also edited the book Cleanroom Design (second edition, 1999). He is a member of British and international standards committees writing the international cleanroom standards. He has extensive experience as an industrial consultant.
He has received the following awards for his work in Cleanroom Technology: Fellowship of the IEST, Honorary Life Member of S2C2, James R Mildon Award from the IEST, Michael S Korczyneski Grant from the PDA (twice), Parenteral Society Annual Award and the CleanRooms Hall of Fame Award.
Preface
The contamination-free conditions provided by cleanrooms are essential for much of modern manufacturing industry. Without cleanrooms, productswill become contaminated and either malfunction or infect people with bacteria. Cleanrooms are used for the manufacture of items used in computers, cars, aeroplanes, spacecraft, televisions, disc players and many other electronic and mechanical devices, as well as the manufacture of medicines, medical devices and foods.
Cleanroom technology can be divided into three parts: design, testing and operation of cleanrooms, and this book covers, in a holistic way, these three main facets. The book is intended to introduce people to these subjects or to update their knowledge. Those who teach ‘cleanroom technology’ either at college, or to their cleanroom personnel, may find this book useful, as it has been written with this in mind.
Most of the principles described in the book are those that are generally accepted within cleanroom industries. However, I have found areas where no sound advice exists and have had to develop guidance using my own knowledge and experience.
The first edition of this book has been well received and translated into several languages. However, new information on cleanrooms is now available and this edition contains a substantial amount of additional material. Each chapter has been updated. This might be by the inclusion of more information, as in the chapter on the history of cleanrooms where information has been added about the early days of infection control in hospitals. However, Chapter 4 and 5, the chapters that contain information on cleanroom standards and guidelines, required extensive updating. Other chapters, such as Chapter 16, which discusses risk management, have also been extensively revised, especially the section on risk assesment. Other subjects that have been added are those on clean-build, determination of air supply volumes for non-unidirectional cleanroom, RABS (Restricted
Access Barrier Systems), contamination recovery test methods, entry of large items into a cleanroom, glove allergy problems, and how to develop a cleanrooom cleaning programme.
I dedicate this book to my sons Griogair and Murray who are both engineers and cleanrooms users.
Acknowledgements
In the first edition of this book I acknowledged the help of (in alphabetical order) Neil Bell, Charles Berndt, Roger Diener, Gordon Farquharson, Gordon King, Lynn Morrison, Bob Peck, Martin Reeves, Hal Smith and Neil Stephenson. I also acknowledged the support of the Scottish Society for Contamination Control. Barbara McLeod read and commented on the script and Isabelle Lawson produced most of the drawings used in both editions of the book.
In preparing the second edition, I asked a number of experts in cleanroom technology to review the chapters that I had rewritten. Don Wadkins supplied information on clean-build contained in Chapter 8. R. Vijayakumar reviewed Chapter 9 on high efficiency air filters. Tim Eaton and Koss Agricola reviewed Chapter 16 on risk management. Roger Diener helped me rewrite Chapter 19 on the materials and the entry of machinery and equipment into a cleanroom. Chapter 20 on cleanroom clothing was revised with the assistance of Charles Berndt. The information on gloves in Chapter 21 was reviewed by Elizabeth Hill. My thanks go to all of these people whose help is much appreciated.
The photographs on the cover of this book are reproduced by permission of Lothian Health Services Archive at Edinburgh University Library, Micronova Manufacturing, International pbi, and Metron Technology. The permission to use other photographs, tables and drawings within the book is acknowledged at the end of each chapter.
Finally, I am most grateful to John Neiger for checking this edition from cover to cover with commendable thoroughness. John combines a considerable knowledge of clean air and containment technology with a passion for clear and understandable writing. This edition of my book has benefited greatly from his input.
1
Introduction
1.1 What is a Cleanroom?
It is clear that a cleanroom is a room that is clean. However, a cleanroom has a special meaning and it is defined in the International Organization for Standarization (ISO) standard 14644–1 as:
room in which the concentration of airborne particles is controlled, and which is constructed and used in a manner to minimise the introduction, generation, and retention of particles inside the room and in which other relevant parameters, e.g. temperature, humidity, and pressure, are controlled as necessary
The first two-thirds of the definition is, in essence, what a cleanroom is. It is a room that minimises the introduction, generation and retention of particles. This is achieved, firstly, by supplying it with an exceptionally large quantity of air that has been filtered with high efficiency filters. This air is used (1) to dilute and remove the particles, bacteria and chemicals dispersed from personnel, machinery and other sources within the room and, (2) to pressurise the room and ensure that no dirty air flows into the cleanroom. Secondly, a cleanroom is built with materials that do not generate particles or ‘outgas’ airborne chemical contamination and can be easily cleaned. Finally, cleanroom personnel use clothing that envelops them and minimises their dispersion of particles and micro-organisms.
A cleanroom with personnel wearing cleanroom clothing

These and other similar measures that minimise the introduction, generation and retention of contamination in a cleanroom are discussed in this book. Cleanrooms can also control the temperature, humidity, sound, lighting, and vibration. However, these parameters are not exclusive to cleanrooms, and are therefore not discussed in any detail in this book.
1.2 The Need for Cleanrooms
The cleanroom is a modern phenomenon. Although the origins of cleanroom design and management go back for more than 150 years and are rooted in the control of bacterial infection in hospitals, the need for a clean environment for industrial manufacturing led to the modern cleanroom in the 1950s. Cleanrooms are needed because people, production machinery and the building structure all generate contamination. As will be discussed later in this book, people and machinery produce millions of particles, and conventional building materials can break up as well as ‘outgas’ chemical contamination. A cleanroom controls the dispersion of all this potential contamination to allow manufacturing to be carried out in a clean environment so that the correct quality and reliability of the product is achieved, and, in the case of healthcare products, the patient is not harmed.
The uses of cleanrooms are diverse and shown in is a selection of products that are now being made in cleanrooms.
Some cleanroom applications
| Industry | Product |
| Electronics | Computers, flat screens |
| Semiconductor | Integrated circuits used in computer memory and control |
| Micromechanics | Miniature bearings, compact-disc players |
| Optics | Lenses, photographic film, laser equipment |
| Nanotechnology | A wide variety of products at nanometre size |
| Biotechnology | Antibiotics, genetically modified organisms (GMOs) |
| Pharmaceutical | Sterile pharmaceuticals |
| Medical Devices | Heart valves, cardiac by-pass systems, stents, catheters |
| Food and Drink | Brewery products, unsterilised food and drink |
It may be seen in that cleanroom applications can be broadly divided into two. Given in the top section of are those industries where dust particles are a problem, and their presence, even in submicrometre size, may prevent a product functioning, or reduce its useful life.
Contaminating particle on a semiconductor
A major user of cleanrooms is the semiconductor fabrication industry, where microprocessors are produced for use in computers, cars and other machines. shows a photomicrograph of a semiconductor with a particle on it. Such particles can cause an electrical short circuit and ruin the semiconductor. To minimise contamination problems, semiconductors are manufactured in cleanrooms with very high standards of cleanliness.
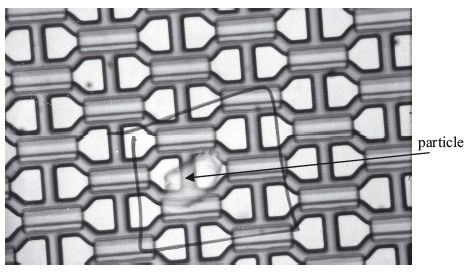
Contaminating particle inhibiting carbon nanotube growth

Shown in is a contamination problem in a nanotechnology application. The photograph shows a particle sitting in the centre of a field of carbon nanotubes that are growing upwards. The growth of nanotubes around the particle is inhibited by chemical contamination diffusing from the particle. Nanotubes beyond the edge of the area of inhibition are seen to have grown normally. In the photograph, the particle is approximately 10 μm micrometres across and the area of inhibition 70 μm in diameter. The nanotubes are only 2 to 3 nanometres in diameter, so are difficult to distinguish one from another. 1 nanometre (nm) = 1/1000 micrometre (μm).
The bottom section of shows manufacturers that require the absence of micro-organisms, as their growth in a product could lead to human infection. The healthcare industry is a major user of cleanrooms, as microorganisms or dirt must not be injected or infused into patients through their products. Hospital operating rooms also use cleanroom technology to minimise wound infection (Figure ).
Unidirectional airflow system and occlusive clothing used in an operating room

It may also be seen from that many of the examples are recent developments and this list will certainly be added to in the future, there being a considerable and expanding demand for this type of room.
1.3 Types of Cleanrooms
Cleanrooms have evolved into two major types and they are differentiated by their method of ventilation. These arenon-unidirectional andunidirectionalairflow cleanrooms. Unidirectional airflow cleanrooms were originally known as ‘laminar flow’ cleanrooms and non-unidirectional flow cleanrooms as ‘turbulently ventilated’. The use of the term ‘laminar flow’ was a mistake, as laminar flow has a meaning in physics and engineering that does not apply to the airflow in a cleanroom. Unidirectional airflow is the correct way of describing the airflow and is the term used in the ISO standards. Unidirectional airflow cleanrooms use very much more air than non-unidirectional airflow cleanrooms, and give superior cleanliness.
Non-unidirectional airflow type of cleanroom

The two major types of cleanroom are shown diagrammatically in Figures and . shows a non-unidirectional airflow cleanroom receiving clean filtered air through a high efficiency air filter and air diffuser in the ceiling. This air mixes with the room air and removes airborne contamination through air extracts at the bottom of the walls. The air change rates are normally equal to, or more than, 20 per hour, this being much greater than in ordinary rooms, such as in offices. In this non-unidirectional style of cleanroom, the contamination generated by people and machinery is mixed with and diluted by the supply air, and then removed.
Unidirectional airflow type of cleanroom
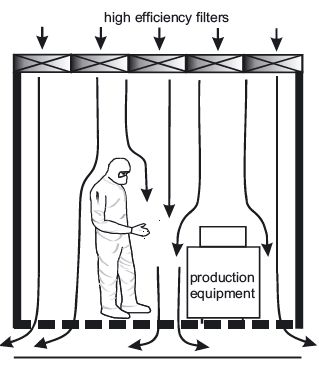
shows the basic principles of a unidirectional airflow room. High efficiency filters are installed across the whole ceiling and the air to the room is supplied through these. This air sweeps down through the room in a unidirectional way at a velocity generally between 0.3 m/s (60 ft/min) and 0.5 m/s (100 ft/min) and exits through the floor, thus removing the airborne contamination from the room. This system uses much more air than the non-unidirectional airflow cleanroom but, because of the directed air movement, it minimises the spread of contamination about the room and sweeps it out through grilles in the floor. An alternative configuration has the high efficiency filters installed across the whole of one wall with the air being removed at the opposite wall.
Separative devices, such as unidirectional airflow benches or isolators, are used in both non-unidirectional and unidirectional airflow cleanrooms. These give a localised supply of filtered air and enhanced air conditions where required, e.g. at the area where the product is open to contamination.
1.4 What is Cleanroom Technology?
Various parts of cleanroom technology and their interconnections
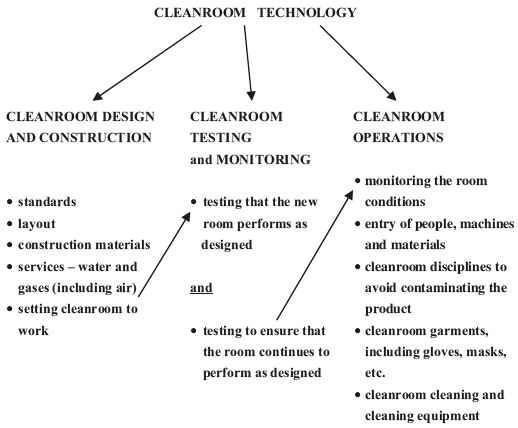
As can be seen in , cleanroom technology can be divided into three broad areas. These areas can also be seen to parallel the application of the technology as the cleanroom user moves from firstly deciding to purchase a room to finally operating it.
Firstly, it is necessary todesign and construct the room. To do this one must consider (1) the design standards that should be used, (2) what design layout and construction materials can be used, and (3) how services should be supplied to the cleanroom.
Secondly, after the cleanroom has been constructed it must betested to check that it conforms to the stipulated design. During the life of the cleanroom, the room must also betested and monitored to ensure that it continually achieves the standards that are required.
Finally, it is necessary tooperate the cleanroom correctly so that the manufactured products are not contaminated. This requires that entry of people and materials, garment selection, cleanroom disciplines and cleaning of the room are all correctly carried out.
These three fundamental elements of Cleanroom Technology are covered in this book.
Acknowledgements
Figure is reproduced by permission of Compugraphics and M+W Pearce. is reproduced by permission of Murray Whyte. is reproduced by permission of Fishers Services.
2
The History of Cleanrooms
2.1 The Earliest Years
Joseph Lister
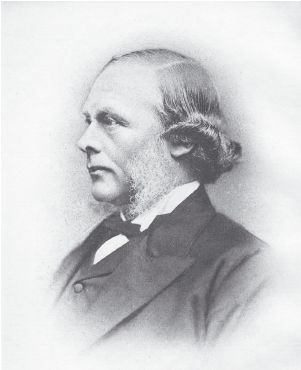
It is clear that the first cleanrooms were found in hospitals. Joseph Lister’s contribution to history was his realisation that bacteria caused surgical wound infection. The discoverer of microbes, Louis Pasteur, wrote that ‘in the field of observations, chance favours the mind that is prepared.’ This is particularly apt when applied to Lister’s discoveries. In 1860 he was appointed Regius Professor of Surgery at Glasgow University. Lister heard of Pasteur’s experiments, which showed that boiling and exclusion of air from meat broth stopped decomposition. Lister realised that this might apply to hospital wounds. He had also read that carbolic acid (the old name for phenol) was being used to decontaminate sewage. The treatment not only suppressed the smell but when the sewage was spread on fields, cows no longer picked up enterozoal infections. In 1865 Lister tried carbolic acid on wounds with great success and in 1867 he used it with similar success in surgery. During surgery he used it on instruments, on the wound and on the surgeon’s hands, and he attempted to prevent airborne infection by spraying it into the air. He found that these steps eliminated many bacteria and reduced infection in the operating room; this was the scientific basis for the first cleanrooms.
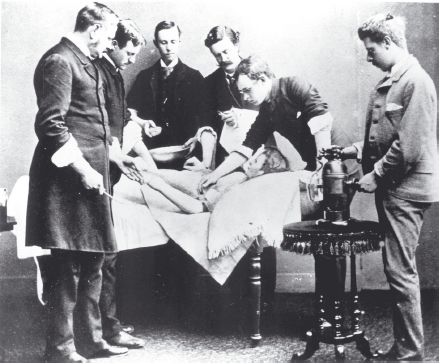
Shown in is a photograph taken in 1889 of a group of surgeons from the Aberdeen Royal Infirmary in Scotland using Lister’s spray, which sprayed carbolic acid into the air of an operating room. This photograph is interesting from several points of view.
Firstly, Lister’s spray is shown and this is of historical interest, although it probably did little to reduce airborne bacteria.
Secondly, shown in is the surgeon Ogston, who is the third figure from the right and famous as the discovery of ‘staphylococci’. Ogston thought that his patient’s abscesses might be caused by bacteria and, using a microscope to look at the pus from abscesses, he found bacteria that had the appearance of either chains or bunches of cocci. When he introduced the pus into animals, abscesses developed with the same type of bacteria as found in the original abscess. He published this information in 1880 and 1881. The type of cocci that grew in chains had already been discovered and named ‘streptococci’ but the type he found in bunches had not and Ogston named them ‘staphylococci’, using the Greek wordstaphyle which means ‘bunch of grapes’. Owing to the golden colour they exhibit when they grew into colonies, he named the bacteriaStaphylococcus aureus. This type of bacteria are still a major cause of infections in hospitals, and in their methicillin resistantStaphylococcus aureus (MRSA) form, they are a major contamination control challenge.
Finally, it is interesting to observe the accepted mode of dress at that time. Although this photograph was probably posed, the clothing worn for actual surgery would have been of the same type, and operations were carried out without the protection of sterile (or even clean) clothing. The frock coat was a standard item of clothing in those days for surgeons and when the coat was too old it ended up in the operating theatre. An operation was a dirty job and a worn old coat was a suitable garment; it was faded with age, stained with blood and spotted with pus. The surgeon might wear an apron or gown, but this would be for the purpose of protecting the surgeon from blood and not the patient from the surgeon’s bacteria.
A group of surgeons with the Lister steam spray (on table).
An operating room in the late 1890s.

A photograph taken in the Royal Infirmary, Edinburgh, Scotland in the 1890s ( ), shows a number of aspects of surgery that will interest anyone who works in a modern cleanroom. The gas lamp seen in the top left-hand side of the picture confirms the age of the photograph, as do many other aspects. The surgeons can be seen to be wearing gowns, but not gloves, hats or masks. In the background of the operating rooms is a gallery where the medical students would crowd in to see the operation without consideration of the bacteria they dispersed; the gallery is the reason that operating rooms are still called operating ‘theatres’ in many parts of the world. The floor is exposed wooden flooring, and the sinks, buckets and exposed pipes reflect a bygone age where little was known about contamination control.
Lister’s reduction of wound sepsis was by anantiseptic method, as he used a disinfectant to kill the bacteria on bandages, the hands of the surgeon and in the operating room environment. One of his former assistants, Sir William Macewen, who succeeded Lister as Professor of Surgery at the University of Glasgow, along with other surgeons in Germany and the USA, developed Lister’s techniques into procedures known asaseptic techniques. These techniques sought not to kill bacteria that entered the wound, but rather to prevent them from getting there in the first place. Boiling of instruments and bandages was introduced and the surgeons and nurses ensured their hands were rigorously ‘scrubbed’ to remove bacteria. By the year 1900, surgical gloves, masks and gowns had been introduced. These could be steam sterilised before an operation, although at a lower temperature and pressure than used today. These methods were the basis of cleanroom techniques in the present.
Shown in is an operating room in the Royal Infirmary, Edinburgh, photographed around 1907. The contrast to the photograph in is very noticeable. Electricity has been installed, but of more interest is the fact that the surgeon is wearing gloves and a facemask. The face mask is below his nose, as it was not till the end of the 1930s that it was appreciated that it should go above the nose. There is also a terrazzo-type floor and tiled walls to facilitate disinfection and cleaning.
Operating room in 1907 showing aseptic precautions

2.2 Ventilated Operating Rooms
Although the operating rooms built before the 1950s had contamination control methods that were similar to modern cleanrooms, an important omission was positive ventilation with filtered air. Artificial ventilation was rarely used in hospitals in temperate climates until the 1940s and then more for comfort than for contamination control. It was only after the end of the 1939-1945 Second World War that ventilation in hospitals was clearly advocated for contamination control. The problems of airborne infection of people in crowded situations that occurred in wartime, e.g. in submarines, air-raid shelters and army barracks, were studied. Microbiological warfare required the airborne dispersion of micro-organisms and this was also studied. In addition, the airborne bacterial sampler was invented, and the ventilation of rooms and the aerodynamics of particles were studied, all during the Second World War.
By the early 1960s, most of the principles that dictate the performance of non-unidirectionally ventilated rooms were known. Also established was the fact that people were the source of airborne bacteria, these being dispersed on skin particles. Open-weave cotton garments did little to prevent this dispersion and tightly woven fabrics were found to be necessary.
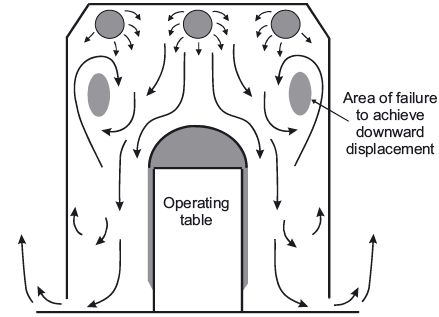
In 1960 Blowers and Crew attempted to obtain a downward ‘piston’ of air (unidirectional airflow, although they did not call it that) from an air diffuser fitted over the entire ceiling in an operating room in Middlesborough, England. Unfortunately, because of the thermal air currents from people and the operating room lamp, as well as movement of people, the low air velocity was disrupted; this made it impossible to achieve good unidirectional airflow. This was the situation when Professor Sir John Charnley (with assistance from Hugh Howorth) decided to improve the ventilation in his operating room at Wrightington Hospital near Manchester in England.
The Charnley-Howorth ‘greenhouse’

Charnley was a pioneer of hip replacement surgery. He devised an operation to replace a diseased joint with an artificial joint made of plastic and metal. His initial operations gave a sepsis rate in the region of 10%. This was a major problem, and so he initiated a number of preventative measures. Using the knowledge that existed at the time (1961), he and Howorth attempted to perfect the ‘piston effect’ of a downward flow of air. Instead of using the whole of the operating room ceiling (as Blowers and Crew had done) they restricted it to a much smaller area and hence improved the downward flow of air. They used a 7 ft × 7 ft ‘greenhouse’ placed within the operating room. This is shown in . shows the diagram Charnley published of the airflow in the ‘greenhouse’; it can be seen that reasonable downward unidirectional airflow was achieved close to the operating table.
Section through Charnley’s original ‘greenhouse’ system showing the airflow
Charnley and Howorth increased the air supply volume and incorporated design improvements using the knowledge gained from work on laminar (unidirectional) airflow systems in the USA and elsewhere. Charnley introduced improvements to the fabric and design of the clothing worn by the operating team to minimise the dispersion of microbes. He found that the improvements to the ventilation of the operating room and the clothing substantially reduced the concentration of airborne bacteria. These reductions were paralleled with reductions in the rate of deep hip infection from about 10% in 1959, when his operating room conditions were poor, to less than 1.0% by 1970 when all his improvements were complete. The Medical Research Council of the United Kingdom confirmed in the 1980s that the use of unidirectional airflow enclosures with occlusive clothing would reduce the rate of joint sepsis to one quarter of that found in conventional non-unidirectional airflow operating rooms.
2.3 Early Industrial Cleanrooms
In engineering industries, similar advances were being made. The development of the first cleanrooms for industrial manufacturing started during the Second World War, mainly in an attempt to improve the quality and reliability of instrumentation used in guns, tanks and aircraft. It was realised that the cleanliness of the production environment had to be improved, or items such as bombsights would malfunction. is a photograph, taken in the nose of a B-17 bomber, of a Norden bombsight that was used in American planes in the Second World War to ensure accurate bombing. As there were gear wheels, ball bearings and a gyroscope that could cause inaccuracies if dirt were introduced, clean conditions were needed for manufacture.
Norden bombsight in the nose of a B-17 bomber

To achieve cleanliness it was assumed that cleanrooms were kept clean like people’s homes. Surfaces like stainless steel, which did not generate particles, were used and kept clean. It was not appreciated that the airborne dispersion of large quantities of particles by machines and people needed to be minimised by supplying large quantities of clean air. For example, the dominant idea in a pharmaceutical production room was that it had to be kept free of microbes by the use of copious quantities of disinfectants. The walls were made suitable for this purpose by being tiled, and the floor would be a terrazzo-type having a gully and drains to remove the disinfectant. Ventilation was very basic, there being few air changes per hour, and there was little in the way of air movement control within the room, or between the production area and outside areas. Personnel were dressed in cotton clothing similar to that used in the operating rooms of that era, and changing areas, if they existed, were very basic.
Work on nuclear fission, as well as biological and chemical warfare research carried out during the Second World War, were the driving forces for the development of High Efficiency Particulate Air (HEPA) filters to contain the dangerous radioactive, microbial or chemical contaminants.
Gyroscope production room at Western Electric

Use of the same type of filters allowed cleanrooms to be supplied with very clean air, and low levels of airborne contamination to be achieved.
Rooms with large volumes of well-filtered air supplied by ceiling diffusers were built between 1955 and the early 1960s. In the early 1950s the Western Electric Company in Winston-Salem, NC, USA was having a major problem in manufacturing missile gyroscopes. About 99 out of 100 gyroscopes were being rejected, the problem being identified as dust. It was decided that a ‘dust-free’ production room should be built and this was designed by the AC Corporation and completed in 1955. shows the room soon after production started.
This may be the first production cleanroom built that recognised all of the basic requirements of a cleanroom. Personnel wore synthetic fabric clothing with a cap; they also had a locker room for changing clothes. Construction materials were chosen for ease of cleaning and to minimise the production of particles. Cracks and corners were minimised, the vinylcovered floors were coved onto the wall and the lighting was flushmounted to minimise dust accumulation. As can be seen in the back righthand side of the photograph, pass-through windows were used. The airconditioned supply was filtered through HEPA or ‘absolute’ filters that were capable of removing 99.95% of 0.3 µm particles, and the room was positively pressurised.
2.4 Unidirectional Airflow Cleanrooms
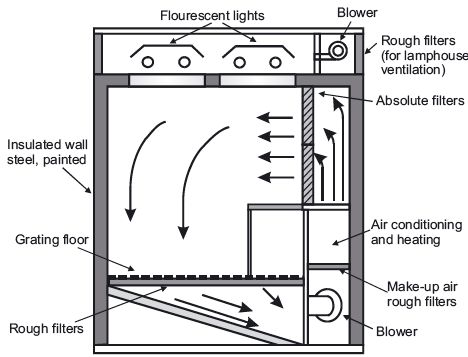
The watershed in the history of cleanrooms was the invention, in 1960, of the ‘unidirectional’ or ‘laminar air’ concept of ventilation at the Sandia Laboratories, Albuquerque, New Mexico, USA. This was a team effort, but it is to Willis Whitfield that the main credit goes. Shown in is a photograph of Willis Whitfield in his original room that was built in 1961.
The room was small, being 6 ft wide by 10 ft long by 7 ft high (1.8 m × 3 m × 2.1 m). Instead of the air being supplied by ceiling diffusers and mixing with the room air in an uncontrolled manner, it was supplied by a bank of HEPA filters. This ensured that air moved in a unidirectional way from the filters, across the room, and out through the floor grilles.
Willis Whitfield in his original laminar air room

Shown in is a cross-sectional drawing of the original unidirectional airflow room. It may be seen that anyone working at the bench in the room should not contaminate anything in front of them, as their contamination would be swept away.
A cross-section of the original unidirectional cleanroom
The invention at Sandia was publicised inTime magazine of April 13th 1962, and this article created a great deal of interest. The article was as follows:
‘Mr Clean
Scientists at the Sandia Corp. in Albuquerque, where nuclear weapons are designed and assembled, have a passion for cleanliness. They have to. As weapons components are made smaller and still smaller, the presence of a single particle of dust can make larger and still larger trouble. The strictest housekeeper in all Sandia is Texas-born Physicist Willis J. Whitfield, creator of the Whitfield Ultra-Clean Room. “I thought about dust particles,” he says with a slight drawl. “Where are these rascals generated? Where do they go?” Once he answered his own questions Physicist Whitfield decided that conventional industrial clean rooms are wrong in principle.
The usual system in clean rooms, which are necessary for an everincreasing number of industrial operations, is to keep dust particles from being released. Smoking is forbidden; so are ordinary pencils, which give off graphite particles. People who work in the clean rooms are “packaged” in special boots, hoods and coveralls and are vacuum-cleaned before they enter. The rooms themselves are vacuumed continually. But despite all these precautions each cubic foot of their air still contains at least 1,000,000 dust particles that are.3 microns (.000012 in.) or larger in diameter. This is a vast improvement over ordinary air, but Whitfield was sure he could do better. Abandoning the idea of keeping dust particles from being generated, he decided to remove them as soon as they appear.
The Whitfield Ultra-Clean Room looks like a small metal house trailer without wheels. Its floor is metal grating. It is lined with stainless steel, and along one wall the workbench faces a 4 ft by 10 ft bank of “absolute filters” that remove all particles above.3 microns from a slow stream of air. Most clean rooms use their filters simply to clean up incoming air. Whitfield’s trick is to make the clean air from the filters keep the room clean. It flows at 1 mph (a very faint breeze) across the workbench and past the people working at it. Workmen can dress in ordinary clothes and smoke if they desire. Dandruff, tobacco smoke, pencil dust and any other particles generated are carried away by the clean air, whisked down through the grating floor, and discharged outdoors. Every six seconds the room gets a change of ultra-clean air. No particles get a chance to circulate, and as a result, Physicist Whitfield’s room is at least 1,000 times as clean as the cleanest of its competitor.’
The concept of unidirectional airflow cleanroom ventilation was very quickly adopted by a large variety of industries, as high-quality cleanrooms were urgently required.
Acknowledgements
is reproduced by permission of Aberdeen City Council, Library and Information Services. and Figures are reproduced by permission of Lothian Health Services Archive, Edinburgh University Library. is reproduced by permission of Howorth Airtech Ltd. is reproduced by permission of British Journal of Surgery. is reproduced by permission of the Conservation Department of the Imperial War Museum, Duxford. The article ‘Mr Clean’ is reproduced by permission of Time Inc.