

Contents
Contributors
Preface
Overview of Practical Guide to Equine Colic
1 Patient Signalment and History
Importance of the patient’s history
Signalment
Obtaining the patient’s history
Application of the patient’s history
2 Physical Examination
Importance of the physical examination
Initial patient observation
Physical examination
Applications of the physical examination
3 Abdominal Palpation per Rectum
Indications
Preparation
Procedure
Complications
4 Nasogastric Intubation
Indications
Preparation
Procedure
Complications
5 Management of Mild Colic
Practical perspective of colic
Clinical indications of mild colic
Management of mild colic
Monitoring
Management changes and prevention
When colic is no longer considered mild
6 Analgesia
Indications
Nonsteroidal anti-inflammatory drugs
Alpha-2 adrenergic agonists
Opioids
Intravenous lidocaine
Hyoscine-N-butylbromide
7 Enteral Fluid Therapy
Indications
Preparation
Technique
Complications
8 Referral of the Horse with Colic
Importance of early referral
Indications
Preparation
9 Clinical Laboratory Data
Indications
Hematology
Clinical chemistry
Coagulation
Application of clinical pathology findings
10 Abdominocentesis and Peritoneal Fluid Analysis
Indications
Preparation
Procedure
Complications
Peritoneal fluid analysis
Application of peritoneal fluid analysis
11 Intravenous Catheterization and Fluid Therapy
Basics of fluid distribution throughout the body
Oxygen delivery to the cells
IV catheterization
IV fluid therapy
12 Abdominal Sonographic Evaluation
Indications
Preparation
Procedure
Application of abdominal sonography to the colic patient
13 Abdominal Radiographic Examination
Indications
Preparation
Procedure
Application of abdominal radiography to the colic patient
14 Trocharization
Indications
Preparation
Procedure
Complications
15 Medical versus Surgical Treatment of the Horse with Colic
General indications for surgery
Indications for specific lesions
The decision for euthanasia without surgical treatment
16 Colic Surgery
Indications
Preparation
Exploratory procedures
Selected surgical procedures
17 Specific Causes of Colic
Gastric diseases
Small intestinal disease
Cecal disease
Large (ascending) colon disease
Small (descending) colon disease
Neoplasia
18 Postoperative Patient Care
Monitoring
Treatment
19 Postoperative Complications
Fever
Ischemia-reperfusion injury
Endotoxemia and SIRS
Diarrhea
Recurrent colic
Postoperative ileus
Septic peritonitis
Postoperative intraperitoneal adhesions
Incisional complications
20 Biosecurity
Importance of biosecurity
Components of a biosecurity program
Biosecurity for the hospitalized equine colic patient
Biosecurity for the equine colic patient at home
21 Special Considerations
Foals
Pregnant mares
Postpartum mares
Colts and stallions
Geriatric horses
Miniature horses, ponies, and donkeys
22 Long-term Recovery and Prevention
Long-term recovery
Prevention
23 Nutrition
Feeding the postoperative colic patient
Long-term nutritional management of the postcolic patient
24 Gastrointestinal Parasitology and Anthelmintics
Gastrointestinal parasitology
Anoplocephala perfoliata
Cyathostomes
Parascaris equorum
Strongylus vulgaris
Anthelmintics
Appendix A Clinical Scenarios
Clinical scenario 1
Clinical scenario 2
Clinical scenario 3
Clinical scenario 4
Clinical scenario 5
Clinical scenario 6
Clinical scenario 7
Clinical scenario 8
Clinical scenario 9
Clinical scenario 10
Appendix B Drug Dosages used in the Equine Colic Patient
Appendix C Normal Ranges for Hematology and Palsma Chemistry and Conversion Table for Units
Index
Advertisements
This book is accompanied by a companion website:
www.wiley.com/go/southwood
The website includes:

This edition first published 2013 © 2013 by John Wiley & Sons, Inc.
Wiley-Blackwell is an imprint of John Wiley & Sons, formed by the merger of Wiley’s global Scientific, Technical and Medical business with Blackwell Publishing.
Editorial Offices
2121 State Avenue, Ames, Iowa 50014-8300, USA
The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK
9600 Garsington Road, Oxford, OX4 2DQ, UK
For details of our global editorial offices, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell.
Authorization to photocopy items for internal or personal use, or the internal or personal use of specific clients, is granted by Blackwell Publishing, provided that the base fee is paid directly to the Copyright Clearance Center,222 Rosewood Drive, Danvers, MA 01923. For those organizations that have been granted a photocopy license by CCC, a separate system of payments has been arranged. The fee codes for users of the Transactional Reporting Service are ISBN-13: 978-0-8138-1832-0/2013.
Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their espective owners. The publisher is not associated with any product or vendor mentioned in this book. This publication is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold on the understanding that the publisher is not engaged in rendering professional services. If professional advice or other expert assistance is required, the services of a competent professional should be sought.
Library of Congress Cataloging-in-Publication Data
Practical guide to equine colic / edited by Louise L. Southwood ; with illustrations by Joanne Fehr.
p. cm.
Includes bibliographical references and index.
ISBN 978-0-8138-1832-0 (hardcover : alk. paper)
1. Colic in horses. I. Southwood, Louise L.
SF959.C6P73 2012
636.1′089755–dc23
2012010995
A catalogue record for this book is available from the British Library.
Wiley also publishes its books in a variety of electronic formats. Some content that appears in print may not beavailable in electronic books.
Cover design by Modern Alchemy LLC
Dedicated to Eric, Aiden, Kody, and Kylie Parente
Scott, Samantha, and Benjamin Fehr
Helen W. Aceto, PhD, VMD
Assistant Professor of Veterinary Epidemiology
Director of Biosecurity
Department of Clinical Studies
New Bolton Center
University of Pennsylvania School of Veterinary Medicine
Kennett Square, Pennsylvania, USA
Jennifer A. Brown, DVM, DACVS
Surgeon
Veterinary Relief, Surgical, and Consulting Services
Tampa, Florida, USA
Sarah Dukti, DVM, DACVS, DACVECC
Surgeon and Emergency/Critical Care Clinician
Piedmont Equine Practice
The Plains, Virginia, USA
Kira L. Epstein, DVM, DACVS, DACVECC
Associate Professor
Department of Large Animal Medicine
College of Veterinary Medicine
University of Georgia
Athens, Georgia, USA
Joanne Fehr, DVM, MS, DACVS
Equine Emergency Clinician
Pilchuck Animal Hospital
Snohomish, Washington, USA
Eileen S. Hackett, DVM, PhD, DACVS, DACVECC
Assistant Professor, Equine Surgery and Critical Care
Department of Clinical Sciences
Colorado State University
Fort Collins, Colorado, USA
Samantha K. Hart, BVMS, MS, DACVS, DACVECC
Lecturer, Large Animal Emergency and Critical Care
Department of Clinical Studies, New Bolton Center
University of Pennsylvania School of Veterinary Medicine
Kennett Square, Pennsylvania, USA
Diana M. Hassel, DVM, PhD, DACVS, DACVECC
Associate Professor, Equine Surgery and Critical Care
Department of Clinical Sciences
Colorado State University
Fort Collins, Colorado, USA
Sarah M. Puchalski, DVM, DACVR
Assistant Professor
Department of Surgical and Radiological Sciences
School of Veterinary Medicine
University of California, Davis
Davis, California, USA
Sarah L. Ralston, VMD, PhD, DACVN
Associate Professor
Department of Animal Science
School of Environmental and Biological Sciences
Rutgers, The State University of New Jersey
New Brunswick, New Jersey, USA
Luiz C. Santos, DVM, MS, DACVA
Research Associate, Large Animal Anesthesia
Department of Clinical Studies
New Bolton Center
University of Pennsylvania School of Veterinary Medicine
Kennett Square, Pennsylvania, USA
JoAnn Slack, DVM, MS, DACVIM
Assistant Professor, Large Animal Cardiology and Ultrasound
Department of Clinical Studies
New Bolton Center
University of Pennsylvania School of Veterinary Medicine
Kennett Square, Pennsylvania, USA
Louise L. Southwood, BVSc, PhD, DACVS, DACVECC
Associate Professor, Large Animal Emergency and Critical Care
Department of Clinical Studies
New Bolton Center
University of Pennsylvania School of Veterinary Medicine
Kennett Square, Pennsylvania, USA
Brett S. Tennent-Brown, BVSc, MS, DACVIM, DACVECC
Senior Lecturer in Equine Medicine
Equine Center
University of Melbourne Veterinary Hospital
Werribee, Victoria, Australia
Raquel M. Walton, VMD, PhD, DACVP
Assistant Professor, Clinical Pathology
Director Clinical Laboratory, MJR-VHUP
Department of Pathobiology
University of Pennsylvania School of Veterinary Medicine
Philadelphia, Pennsylvania, USA
Practical Guide to Equine Colic follows the management of a colic patient from obtaining the history and performing a physical examination through to long-term recovery and an attempt at describing prevention. There are several books available with details of the gastrointestinal anatomy and physiology and the objective of this book was not to duplicate these publications but to present the practical aspect of this information. Our focus as equine veterinarians should be to provide the best possible care for our patients and service to our clients by having up to date knowledge to enable us to best diagnose, treat, and prevent disease. We also have the responsibility to educate the next generation of veterinarians, teach each other by sharing our experience, and to continue to investigate disease processes in order to improve management and prevention. Fiscal responsibility has become increasingly important in recent years. We now more than ever need to weigh the benefit against the expense of a particular diagnostic test or treatment and keep costs in a range where clients can afford to treat their animal while being able to maintain a successful practice. We hope that the book and website will be a useful resource for education of veterinary students, interns, and residents, and provide continuing education for experienced equine practitioners. We encourage equine specialists to use the book and website for teaching and identification of knowledge gaps that should stimulate research ideas to improve equine colic patient management. I personally learned a considerable amount researching the literature to prepare the chapters and reviewing the chapters written by the other authors. While not specifically written for horse owners, the information provided particularly on specific diseases and colic surgery may be of interest to the inquisitive and educated lay-person.
A team-approach was essential for successful completion of this project. When asked by Wiley-Blackwell to write a small 200-page book about equine colic, it seemed like a reasonable endeavor. Thinking I knew something about colic but probably not enough to cover 200 pages (even with large print and a lot of pictures), I sought out several colleagues with expertise in specific areas. I am extremely grateful for the contributing efforts of the chapter authors and the book would not have been feasible without these exceptional veterinarians. Dr. Joanne Fehr, a fellow surgical resident and friend, provided illustrations which give considerable educational value to the material. In all honesty, the chapters would still be in draft form buried somewhere on my desk if it wasn’t for Ms. Susan Engelken at Wiley-Blackwell being relentless with ensuring deadlines were met (give or take several months) and my family for giving me the time to meet those deadlines. And we would like to thank the IT support staff at Penn Vet's New Bolton Center, particularly Mr. Tyler Harold, Ms. Linda Lewis, and Mr. Ryan Delaney, for their assistance with video production. Our hope is that this book, which of course is well beyond 200 pages, improves the care of colic patients and the service provided to horse owners through education of equine veterinarians.
The book follows through the basic management of a horse with colic from initial examination (history and physical examination in dark gray) through to long-term recovery and prevention measures including nutritional and parasite management (light olive green). Diagnostic tests are in purple and procedures are in green. The points when these diagnostic tests and procedures are typically performed throughout the course of management are indicated. The key areas of colic patient management (management of mild colic, sedation and analgesia, enteral and intravenous fluid therapy, surgery, and postoperative care including nutrition and postoperative complications) are in orange. It is important to keep in mind that most horses with colic have what is generally considered to be gas colic and will respond to a single dose of flunixin meglumine (or other analgesic) with or without enteral fluids or mineral oil. However, early recognition of the need for referral or surgical intervention is important. Decision-making points (i.e., referral and surgery) are in light gray. Typical lesions seen in horses with colic and special considerations for equine patients with colic of a specific signalment (i.e., specific causes of colic and special considerations) are shown in pink. Because of the importance of infection as a postoperative complication, there is a section on biosecurity. Clinical scenarios illustrating points throughout the text are in Appendix A; dose rates for drugs used in the management of colic patients are in Appendix B; and reference ranges for laboratory data as well as conversion tables for conventional and SI units are in Appendix C. And we would like to thank the IT support staff at Penn Vet’s New Bolton Center, particularly Mr. Tyler Harold, Ms. Linda Lewis, and Mr. Ryan Delaney, for their assistance with video production.
Quizzes for each chapter, additional clinical scenarios, and video demonstrations of surgical procedures are available online at www.wiley.com/go/southwood.

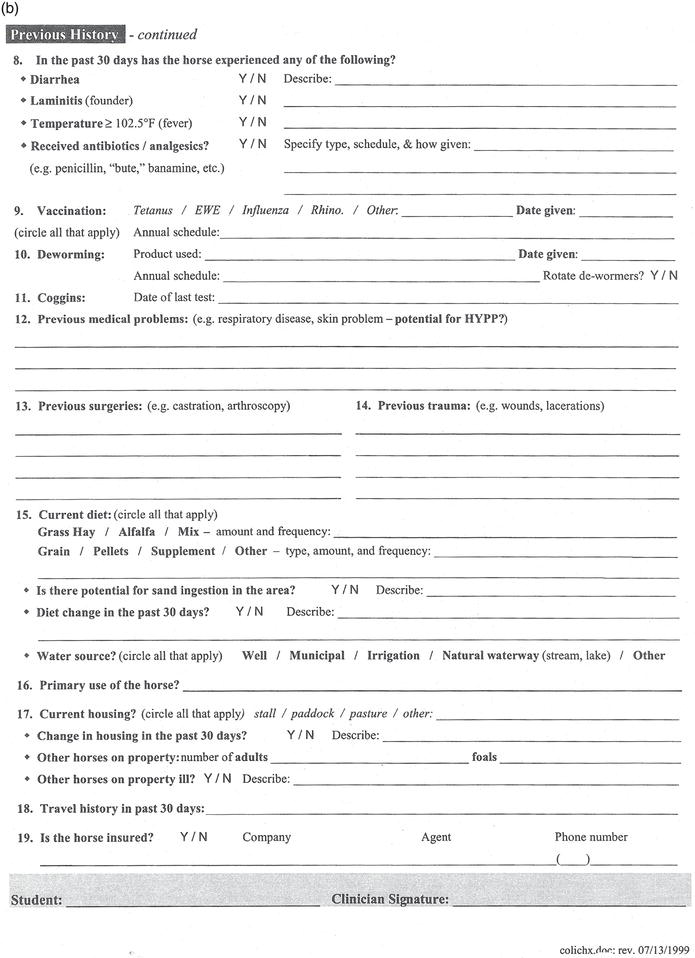
Obtaining a detailed history provides information that can be used to formulate a differential diagnosis list for the horse with colic, direct treatment, and devise a colic prevention plan. Having a standardized history sheet (Figure 1.1) as part of the medical record will streamline the history-taking procedure and ensure details are not omitted. Recording the history as part of the medical record is also important to provide accurate information for referral, for reference in the case of future colic episodes, and as part of a preventative medicine program.
Figure 1.1 Example of a detailed patient history sheet. (a) Front and (b) back.
Source: Courtesy of Colorado State University, Fort Collins, Colorado.

Knowledge of the patient’s signalment, namely, age, breed, and gender, is extremely important during evaluation for colic. While gas colic is by far the most common diagnosis across most age, breed, and gender categories,28 the signalment is critical for forming a differential diagnoses list. Gas colic can be defined clinically by horses with mild to moderate pain that resolves spontaneously or with a single dose of an analgesic drug and accounts for about 70–80% of colic episodes.28 Typical differential diagnoses for equine patients of various signalments are shown in Table 1.1.
Signalment is also important because it may direct the history-taking process. For example, (1) if you are presented with a mare showing colic signs, the reproduction status requires investigation; (2) if you have an older horse, underlying diseases should be considered; and (3) in the case of a neonate, questions pertaining to parturition, passive transfer of maternal antibodies, and clinical signs shown by other foals on the farm should be asked. Specific questions are addressed below.
Table 1.1 Differential diagnoses other than gas colic for patients of a specific signalment.
| Signalment | Differential diagnoses |
| Neonate (p. 279) |
|
| Geriatric horse (p. 286) |
|
| Pregnant mare (p. 282) |
|
| Postpartum mare (p. 284) |
|
| Stallion (p. 285) |
|
| Miniature horse (p. 287) |
|
| Yearling |
|
| Weanling (p. 280) |
|
Obtaining a thorough and accurate yet succinct patient history is one of the most important and perhaps one of the more difficult aspects of evaluating the colic patient (Table 1.2). It involves asking a few initial key questions of the owner/caregiver, keeping the owner/caregiver focused on answering the questions thoroughly and concisely during an often stressful situation, and then recognizing areas of the patient’s history that require a more in-depth discussion that may take place following the examination.
Table 1.2 Pertinent questions to be asked of the owner/caregiver for the equine colic patient.
Initial history
Appetite, water consumption, defecation, urination
Management
Medical history
|
Meticulous medical records need to be maintained with the historical information. Having a standardized history sheet for horses with colic can assist in obtaining a complete history with each case. Further, owners may be able to complete some parts of the history form while the physical examination is being performed (Figure 1.1).
While history taking is traditionally incorporated into the first part of the patient evaluation, it is important to recognize that the entire history does not need to be obtained prior to examining the patient particularly if the patient is showing severe colic signs. However, there are a few very pertinent historical facts that may alter your initial approach to patient care:
The owner/caregiver should be able to describe specifically the signs being demonstrated by the horse or foal. The term “colic” is often used to describe any equine patient that is “not quite normal“. Recumbency and signs of dull mentation and inappetence are often described as colic. While these signs may be associated with colic, other disease processes should also be considered. Persistent recumbency is more typical of a horse with neurological disease (e.g., equine herpes virus, botulism, or cervical spinal cord injury), severe laminitis, trauma with musculoskeletal injury, debility, or shock from other causes (e.g., blood loss). Dull mentation and inappetence can be associated with any systemic disease process (e.g., colitis, pleuropneumonia, hepatic or renal disease) as well as problems of the head and neck regions.
Signs specific for the horse with colic include pawing at the ground, flank staring, kicking at the abdomen, and rolling. If the horse is not showing any of these signs, the horse is likely to have another problem rather than colic. Colic signs are often described as mild, moderate, or severe:
Clinical signs shown by the horse should also be interpreted with regard to any analgesic medication (i.e., flunixin meglumine, phenylbutazone, meloxicam, firocoxib) the owner may have administered to the horse that may alter the degree of pain.
The change in clinical signs over time should also be noted, for example, horses with large colon volvulus (p. 220) may have a history of several hours of mild to moderate colic that has recently become markedly more severe; horses with a nephrosplenic ligament entrapment (NSLE) (p. 219) often have periods of moderate pain intermixed with periods of comfort; a horse with an ileocecal intussusception (p. 213) may have a history of chronic intermittent colic with an acute colic episode; and horses with gastric or cecal rupture (p. 206, 215) may have had a history of variable degrees of pain that has progressed to no further signs of pain and shock (sweating, muscle fasciculations, reluctance to move). See Chapter 2 on Physical Examination (p. 12) for further discussion on pain assessment.
While the owner/caregiver can rarely give an accurate time of when the colic signs actually began, they should be able to tell you (1) when the signs were first observed and (2) when the horse or foal was last observed to be normal. Knowledge of at least an approximate duration of signs is important when performing a differential diagnosis list, for example, mild colic for 24 h may indicate a large colon impaction (p. 217) whereas a strangulating lesion (p. 209, 220) may be higher on the differential diagnosis list for horses showing acute severe colic for 1–3 h despite administration of analgesia.
Duration of colic is also vital for determining a diagnostic and treatment plan including the use of diagnostic tests such as abdominal sonographic and radiographic examination in horses with chronic intermittent colic signs, route of fluid therapy (e.g., a horse with a prolonged duration of colic may benefit from intravenous (IV) fluids), and whether or not to refer the horse or manage the horse surgically versus medically (e.g., a long duration of moderate colic that is unresponsive to analgesia is more likely to require surgical management). While other clinical findings, such as heart rate and packed cell volume, are likely more predictive, duration of colic can provide the owner with some information pertaining to prognosis.
Knowledge of a mare’s reproductive status is critical because management of colic in periparturient mares can be particularly challenging from a diagnostic and therapeutic perspective. Specific questions pertaining to the pregnant mare are in Table 1.3. See Chapter 21 on Special Considerations (p. 278).
Whether or not the horse has been eating, drinking, defecating, and urinating can provide an overall impression of general well-being of the patient. This information may not be available if the horse resides at pasture, particularly if the horse is at pasture with other horses.
The owner/caregiver should be asked about the horse’s recent feed intake, whether or not the horse’s appetite has been normal and whether or not the horse has been drinking an acceptable volume of water.
Table 1.3 Specific history questions pertaining to the broodmare.
|
Nutritional needs of horses are extremely variable and observation of body condition score (p. 15) is likely the best way to determine the adequacy of nutrition. Whether the horse’s appetite has changed and any associated changes in body condition as well as the period of time over which this has occurred are important to note.
Water consumption is variable and dependent on the body weight of the horse, ambient temperature, type of feed (i.e., higher water consumption with hay compared to pasture), activity level, and reproductive status (i.e., pregnancy and in particular lactation increase water requirements). Typically, an adult horse will consume 35–70 L of water a day or about 7–15% of their body weight. Horses require 2–3 L of water per kilogram of dry feed intake. See also Water source.
The last observed defecation amount (e.g., several piles overnight) and consistency (e.g., firm and dry vs. soft or liquid) should be noted. Normal fecal output in an adult horse is 6–8 piles of soft to firm formed feces a day. Whether or not the horse has been observed to urinate or there were several wet areas in the stall should be determined and used to assess hydration status and renal function.
Type of feed provided, method of feeding, frequency of feeding, and if there has been any change in feeding regimen should be ascertained and may be related to the colic signs.2
Specific hay types have been associated with certain types of colic: Coastal Bermuda grass hay that is fed in the southeastern USA has a strong association with ileal (p. 208)17 and possibly cecal (p. 214) impactions; enterolithiasis (p. 218) has been associated with feeding alfalfa hay;7,10,11 and poor quality hay and hay in round bales have been associated with colic.13,14 Other examples of relationship between feed type and colic include the association between colic and feeding high levels of concentrate (e.g., >2.5kg/day dry matter),6,14,29 which alters the contents of the colon and may increase tympany and colonic displacements;18 equine gastric ulcer syndrome and high concentrate diets;4 and sand colic (p. 217) that has been associated with feeding on the ground in areas with sandy soil (e.g., Arizona, California, Colorado, Delaware, Florida, Michigan, and New Jersey).
Horses typically graze for about 18 h each day and management practices of many horses do not necessarily mimic the horses’ natural grazing habits. Many studies on colic have found an association between colic and less pasture time.12,13,29 Alteration in diet and feeding practices (e.g., more time at pasture) may be necessary to manage gastrointestinal problems in some horses.
In several studies, an association between change in feed or feeding regimen and signs of colic has been identified.3,6,12,13,29 Supporting these findings is the overall higher incidence of colic in the spring and possibly autumn months that tend to be associated with a change in feed particularly for pasture-fed horses.3,30 Therefore, any change in diet should be made gradually in an attempt to avoid colic signs.
Dental care is also thought to be important in the prevention of colic with an increasing time from last dental care being associated with colonic impactions.12
The water source should be determined, for example, stream, pond, or water bucket. Access to ponds is associated with a decreased risk of colic compared to other water sources.5 A decrease in water consumption14 or lack of access to water24 is also associated with colic. Owners should be aware of the potential consequences of a freezing water source during the winter months. During autumn and winter and early spring, the water source may not necessarily freeze but become cold. Water temperature was found to affect consumption during cold but not hot weather.16,21 During cold weather, horses with only warm water available drink a greater volume each day than if they have only icy cold water available; however, if they have a choice between warm and icy water simultaneously, they drink almost exclusively from the icy water and drink less volume than if they have only warm water available. While the higher incidence of horses with small (p. 221) and large colon (p. 217) impactions during the winter months3 may be associated with housing and diet, inadequate water intake during these months may also be a contributing factor. Mineral content of water should also be considered in areas where horses are predisposed to enterolithiasis.10,11 All horses should have a readily available source of fresh, palatable water available and water intake monitored when possible.
An increase in the number of hours in a stall and decrease in exposure pasture and recent change in exercise regimen increased the risk for colic and simple colonic obstruction and distention.12,13 Horses that are housed for 19–24 h a day are at a particular risk for colic compared to horses at pasture.5,6,12,13 On the other hand, access to pasture and duration of access have been associated with increased risk of equine grass sickness (p. 209) in certain geographical regions.20 Large colon (p. 217) and cecal (p. 214) impaction are particularly associated with recent stall confinement. For example, a horse that is normally in the pasture and is stall confined because of an injury is predisposed to cecal impaction. Appetite and fecal output should be monitored closely in these horses.
Recent transportation has been associated with colic. Horses that had a history of travel in the previous 24 h had an increased risk of simple colonic obstruction and distention compared to horses that had not been transported.12 Stress, change in diet and water consumption, and possibly restricted movement are likely related to the association between travel and colic. Horses may come into contact with infectious disease during transportation particularly in association with shows or events. There has been also been an association between transportation and salmonellosis: (1) transportation had a major role in reactivating Salmonella sp. infection in carrier ponies22 and (2) horses with a travel time to the hospital >1 h were at an increased risk for shedding salmonella compared to horses with a shorter travel time.15
While there may not be an association between geographical region and occurrence of colic,30 specific types of colic tend to occur in different regions:
It is, therefore, important to know where the horse has previously resided as well as when and for how long the horse was in that region.
Detailed information is in Chapter 24 on Gastrointestinal Parasitology and Anthelmintics (p. 316). The history of anthelmintic therapy needs to be obtained including the anthelmintic(s) used, frequency of administration, and results of monitoring of parasite burden.
While historically Strongylus vulgaris (large red worm) was associated with colic, with the development of ivermectin-based anthelmintics the role of S. vulgaris in colic has diminished.2 Anoplocephala perfoliata (tapeworms) have been associated with many forms of colic including gas colic (p. 45), ileal impaction (p. 208), ileocecal, cecocecal, and cecocolic intussusceptions (p. 213, 214), and cecal impaction (p. 214).2,19,23 Therefore, treatment with praziquantel tartrate or pyrantel pamoate should be part of the anthelmintic regimen. Cyathostomes (small red worms) have been associated with large colon lesions2,31 and Parascaris equorum (round worms) have been associated with intestinal obstruction, rupture, peritonitis, intussusception, or abscessation in foals.2,25 Monitoring of resistance of these parasites to routinely used anthelmintics such as ivermectin is recommended.
Horses that were not treated with an ivermectin- or moxidectin-based anthelmintic within the previous 12 months12 or were not on a regular deworming program6 were predisposed to colic and horses recently administered an anthelmintic were at a decreased risk of colic.13 Recent anthelmintic administration, however, within 7–8 days was associated with colic6 and ascarid impaction.25
Vaccination history is also important particularly in cases where it may not be clear that the horse is showing signs of colic. Diseases for which clinical signs can be mistaken for colic and vaccination is available include botulism, rabies, and other neurological diseases. There has only been one study associating vaccination (Potomac horse fever) with colic signs.20 Research is currently being undertaken to determine the possibility of an equine grass sickness vaccine.29
Horses that have had previous colic surgery and previous episodes of colic are predisposed to colic.5,6,12,24,29,30 Horses with a large colon volvulus and displacement necessitating surgical correction were significantly more likely to colic after surgery if they had more than one episode of colic prior to the one necessitating surgery.26,27
The specific diagnosis and procedure performed during a previous colic surgery often provides an indication of the cause of colic: for example, colonic displacements (NSLE and right dorsal displacement) and large colon volvulus have a tendency to recur; horses with small intestinal and small colon lesions are predisposed to adhesions; and a previous history of jejunocecostomy may be associated with stenosis at the site of an anastomosis. Often owners/caregivers may be aware of previous colic or colic surgery but with no knowledge of the cause. Owners/caregivers should be encouraged to keep records of the horses under their care so that this information is readily available to the attending veterinarian.
The frequency and severity of previous colic episodes should be recorded. Recurrent intermittent colic warrants a more in-depth diagnostic workup including gastroscopy, radiography (p. 149, e.g., sand or enterolithiasis), sonographic examination (p. 116), and abdominocentesis (p. 87, e.g., neoplasia).
Knowledge of current or recent medication including dose rate, route, and frequency of administration that the horse is or was receiving is critical so that
There are certain causes of colic associated with a particular medical history. Acute colitis should be considered in horses with a history of antimicrobial drug administration. Horses with colitis can initially show signs of colic that progress to dull mentation and diarrhea. Colitis should be considered particularly in horses with a fever. Cecal impaction should be considered in horses with a history of recent surgery or stall confinement for an injury. Recent lameness has been associated with colonic impaction.12
Whether or not the owner has administered any medication for the current episode of colic, including the route of administration, dose rate, and frequency, should be noted.
Knowledge of recent medical problems of other horses stabled at the same location may be useful to determine a diagnosis and assist with recommendations for prevention and treatment: for example, in the case where several animals have had problems with colic following treatment with the licicide amitraz; on a farm that has had a problem with strangles, abdominal abscessation should be considered; ileocecal intussusception should be considered on farms with a suspected high incidence of tapeworm infection; and sand colic should be suspected in horses residing in areas particularly if there is a problem with sand colic on the farm.
Stable vices, such as crib biting or windsucking, have been recently associated with colonic colic9 and epiploic foramen entrapment.1
Clinical scenarios 1–3, located in Appendix A, are examples of cases where case history is important in determining a tentative diagnosis and case management. Further discussion on the integration of patient history into case management is included in Chapter 8 on Referral of the Horse with Colic (p. 71) and Chapter 15 on Medical versus Surgical Treatment of the Horses with Colic (p. 164). Quizzes for each chapter, additional clinical scenarios, and video demonstrations of surgical procedures are available online at www.wiley.com/go/southwood.
References
1. Archer. D.C., Freeman, D.E., Doyle. A.J., Proudman, C.J. & Edwards, G.B. (2004) Association between cribbing and entrapment of the small intestine in the epiploic foramen in horses: 68 cases (1991–2001). Journal of the American Veterinary Medical Association, 15, 562–564.
2. Archer, D.C. & Proudman, C.J. (2006) Epidemiolical clues to preventing colic. The Veterinary Journal, 172, 29–39.
3. Archer, D.C., Pinchbeck, G.L., Proudman, C.J. & Clough, H.E. (2006) Is equine colic seasonal? Novel application of a model based approach. BMC Veterinary Research, 2, 27.
4. Buchanan, B.R. & Andrews, F.M. (2003) Treatment and prevention of equine gastric ulcer syndrome. Veterinary Clinics of North America: Equine Practice, 19, 575–597.
5. Cohen, N.D., Matejka, P.L., Honnas, C.M. & Hooper, R.N. (1995) Case-control study of the association between various management factors and development of colic in horses. Texas Equine Colic Study Group. Journal of the American Veterinary Medical Association, 206, 667–673.
6. Cohen, N.D., Gibbs, P.G. & Woods, A.M. (1999) Dietary and other management factors associated with colic in horses. Journal of the American Veterinary Medical Association, 215, 53–60.
7. Cohen, N.D., Vontur, C.A. & Rakestraw, P.C. (2000) Risk factors for enterolithiasis among horses in Texas. Journal of the American Veterinary Medical Association, 216, 1787–1794.
8. Edwards, G.B. (2000) Duodenitis-proximal jejunitis (anterior enteritis) as a surgical problem. Equine Veterinary Education, 12, 318–321.
9. Freeman, D.E. (2000) Duodenitis-proximal jejunitis. Equine Veterinary Education, 12, 322–332.
10. Hassel, D.M., Langer, D.L., Snyder. J.R., Drake, C,M., Goodell, M.L. & Wyle, A. (1999) Evaluation of enterolithiasis in equids: 900 cases (1973–1996). Journal of the American Veterinary Medical Association, 15, 233–237.
11. Hassel, D.M., Aldridge, B.M., Drake, C.M. & Snyder, J.R. (2008) Evaluation of dietary and management risk factors for enterolithiasis among horses in California. Research in Veterinary Science, 85, 476–480.
12. Hillyer, M.H., Taylor, F.G., Proudman, C.J., Edwards, G.B., Smith, J.E. & French, N.P. (2002) Case control study to identify risk factors for simple colonic obstruction and distension colic in horses. Equine Veterinary Journal, 34, 455–463.
13. Hudson, J.M., Cohen, N.D., Gibbs, P.G. & Thompson, J.A. (2001) Feeding practices associated with colic in horses. Journal of the American Veterinary Medical Association, 219, 1419–1425.
14. Kaya, G., Sommerfeld-Stur, I. & Iben, C. (2009) Risk factors of colic in horses in Austria. Journal of Animal Physiology and Animal Nutrition, 93, 339–349.
15. Kim, L.M., Morley, P.S., Traub-Dargatz, J.L., Salman, M.D. & Gentry-Weeks, C. (2001) Factors associated with Salmonella shedding among equine colic patients at a veterinary teaching hospital. Journal of the American Veterinary Medical Association, 218, 740–748.
16. Kristula, M.A. & McDonnell, S.M. (1994) Drinking water temperature affects consumption of water during cold weather in ponies. Applied Animal Behaviour Science 41, 155–160.
17. Little, D. & Blikslager, A.T. (2002) Factors associated with development of ileal impaction in horses with surgical colic: 78 cases (1986–2000). Equine Veterinary Journal, 34, 464–468.
18. Lopes, M.A., White, N.A. 2nd, Crisman, M.V. & Ward, D.L. (2004) Effects of feeding large amounts of grain on colonic contents and feces in horses. American Journal of Veterinary Research, 65, 687–694.
19. Mair, T.S., Sutton, D.G.M. & Love, S. (2000) Caecocaecal and caecocolic intussusceptions associated with larval cyathostomosis in four young horses. Equine Veterinary Journal, 32, 77–80.
20. McCarthy, H.E., Proudman, C.J. & French, N.P. (2001) The epidemiology of equine grass sickness—A literature review (1909–1999). The Veterinary Record, 149, 293–300.
21. McDonnell, S.M. & Kristula, M.A. (1996) No effect of drinking water temperature on consumption of water during hot summer weather in ponies. Applied Animal Behaviour Science 49, 149–163.
22. Owen, R.A., Fullerton, J. & Barnum, D.A. (1983) Effects of transportation, surgery, and antibiotic therapy in ponies infected with Salmonella. American Journal of Veterinary Research, 44, 46–50.
23. Proudman, C.J., French, N.P. & Trees, A.J. (1998) Tapeworm infection is a significant risk factor for spasmodic colic and ileal impaction colic in the horse. Equine Veterinary Journal, 30, 194–199.
24. Reeves, M.J., Salman, M.D. & Smith, G. (1996) Risk factors for equine acute abdominal disease (colic): Results from a multi-centre case-control study. Preventive Veterinary Medicine, 26, 285–301.
25. Southwood, L.L., Ragle, C.A., Snyder, J.R., et al. (2002) Surgical treatment of ascarid impactions in foals and horses. In: Proceedings of the Seventh Equine Colic Research Symposium, Manchester, U.K., pp. 112–113.
26. Southwood, L.L., Bergslien, K., Jacobi, A., et al. (2002) Large colon displacement and volvulus in horses: 495 cases (1987–1999). In: Proceedings of the Seventh Equine Colic Research Symposium, Manchester, U.K., pp. 32–33.
27. Southwood, L.L. (2006) Acute abdomen. Clinical Techniques in Equine Practice, 5, 112–126.
28. Tinker, M.K., White, N.A., Lessard, P., et al. (1997) Prospective study of equine colic incidence and mortality. Equine Veterinary Journal, 29, 448–453.
29. Tinker, M.K., White, N.A., Lessard, P., et al. (1997) Prospective study of equine colic risk factors. Equine Veterinary Journal, 29, 454–458.
30. Traub-Dargatz, J.L., Kopral, C.A., Seitzinger, A.H., Garber, L.P., Forde, K. & White, N.A. (2001) Estimate of the national incidence of and operation-level risk factors for colic among horses in the United States, spring 1998 to spring 1999. Journal of the American Veterinary Medical Association, 219, 67–71.
31. Uhlinger, C. (1990) Effects of three anthelmintic schedules on the incidence of colic in horses. Equine Veterinary Journal, 22, 251–254.
Being able to perform a good physical examination is paramount when examining the colic patient. While recent focus has been on more advanced laboratory and imaging diagnostic tools such as blood and peritoneal fluid lactate concentration (p. 81, 92) and abdominal sonographic examination (p. 116), the physical examination along with obtaining a thorough patient history remains the cornerstone of good veterinary medicine.
Information obtained during physical examination of the colic patient is used to confirm that the horse has colic and determine the severity and possible cause, direct analgesic and fluid therapy, make decisions with regard to medical or surgical treatment, and provide the owners with some indication of prognosis.
Meticulous medical records are necessary when examining the horse with colic (Figure 2.1). Often the examination is performed on an emergency basis and at a time of day that is less than convenient. Expecting to recall findings at a later time is unreasonable, at least for most veterinarians. Recording physical examination findings is important so that trends over time can be observed, all abnormal findings can be noted and a problem list formed, and information can be accurately and completely communicated if referral becomes necessary. Should the horse have recurrent bouts of colic, comparison of physical examination findings on each occurrence can be made and trends identified.
Examining the colic patient begins with making several observations during the approach to the horse or foal. The cardiovascular status should be examined first followed by a more thorough examination of pertinent body systems. A checklist of key observations and physical examination findings for the colic patient are provided in Table 2.1.
Patient examination begins with a careful 30–60 s observation (Table 2.1). Particular attention should be paid to the horse’s body condition (Table 2.2). Poor body condition may be an indication of an underlying disease process (e.g., neoplasia, hepatic or renal disease, right dorsal colitis), inadequate nutrition, or poor dentition.
Mentation or attitude is described as bright, alert, and responsive; quiet and alert; dull or obtunded. Horses with colic are generally bright and alert and will be attentive and even vocalize during the veterinarian’s approach. On the other hand, horses with colitis, proximal enteritis (PE), or peritonitis including gastrointestinal rupture tend to have a dull mentation. Abnormal mentation should also be considered with some neurological disease or toxicity. Assessment of mentation should take into consideration any history of the horse being administered a sedative/analgesic drug.
Evidence of inappropriate sweating can be an indication of severe pain or shock. Other disease processes such as equine protozoal myeloencephalitis (EPM) or pituitary pars intermedia dysfunction (Cushing’s Disease), can cause inappropriate sweating but should only be considered with other signs that do not fit with colic.