

Contents
Contributors
Foreword
Acknowledgements
Abbreviations
Section 1: Anatomy and Function
1 The Normal Anatomy of the Osseous Structures of the Back and Pelvis
Introduction
Vertebral numbering system
Standard vertebral formula
Variations in the vertebral formula
Transitional vertebrae
Developmental aspects and growth plate closure times
Structure of the thoracic and lumbar vertebrae
Vertebral bodies
Intervertebral discs
Vertebral arch
Intervertebral foramina
Lateral foramina
Sacral foramina
Vertebral canal contents
Dorsal spinous processes
Articular processes (facets)
Transverse processes
Lumbosacral junction
Sacrum
Sacroiliac joint
Articulations of the vertebral column
The pelvis
Coccygeal vertebrae
References
2 The Normal Anatomy of the Soft Tissue Structures of the Thoracolumbar Spine
Introduction
Musculature
Ligaments
Reference
3 The Normal Anatomy of the Soft Tissue Structures of the Pelvis
Introduction
Sacroiliac joint
The dorsolateral and caudal walls
The ventral fibrous structures
Conclusion
References
4 The Normal Anatomy of the Nervous System
Introduction
The vertebral column and spinal cord segments
The spinal nerves
The sensory system
The motor system
Distribution of the spinal nerves of the back and pelvis
Sympathetic innervation
Lumbosacral plexus
Conclusion
References
5 Kinematics of the Equine Back
Introduction
Historical perspective
Biomechanical models of how the equine back works
Kinematics of the equine back – ex vivo research
Kinematics of the equine back – in vivo research
Applied kinematics of the equine back
Therapeutic or diagnostic interventions
Effect of clinical pathology
Conclusions and possible future developments
References
Section 2: The Investigation of Back Pathology
6 The Clinical Examination
Introduction
Factors that might complicate the clinical examination
The purpose of the clinical examination
Primary back pain versus secondary back pain
The clinical examination
Ancillary clinical aids
References
7 The Neurological Examination
Introduction
History
Examination at rest
Local reflexes
Areas of sweating
Examination of posture and gaits
Conclusion
References
8 Radiography
Introduction
Indications for radiography of the back and/or pelvis
Technical difficulties with radiography of the equine back and pelvis
Radiographic technique
Positioning and radiograph acquisition
Normal radiographic appearance of the back
An introduction to radiographic abnormalities of the back and pelvis
References
9 Nuclear Scintigraphy
Introduction
Indications for nuclear scintigraphy of the back and/or pelvis
Mechanism of action
Procedure for scintigraphy of the back and pelvis
The normal scintigraphic appearance of the back and pelvis in the horse
Scintigraphic abnormalities of the back and pelvis
Limitations in the use of nuclear scintigraphy in the vertebral column and pelvis
References
10 Ultrasonography of the Thoracolumbar Region
General considerations
SSL and ISL ultrasonography
Ultrasonography of the DSPs
Ultrasonography of the “articular facets” – the articular process–synovial intervertebral articulation
Conclusion
References
11 Ultrasonography of the Lumbosacral Spine and Pelvis
Introduction
Lumbar spine and sacroiliac region
Transcutaneous evaluation
Further reading
12 Thermography
Introduction
Instrumentation
Principles of use
Use in veterinary medicine
Thermography of the back
Conclusions
References
Section 3: The Diagnosis and Treatment of Specific Conditions
13 Traumatic Damage to the Back and Pelvis
General principles
Fracture of the dorsal spinous processes of the thoracic vertebrae (fractured withers)
Fractures of the thoracolumbar vertebral column
Pelvic factures
Prognosis and treatment
References
14 Overriding Dorsal Spinous Processes
Anatomy of the dorsal spinous processes
Incidence
Pathogenesis
Site of pathology
History
Clinical examination
Diagnosis
Diagnosis of anatomical abnormalities
Treatment
Conclusion
References
15 Miscellaneous Osseous Conditions
Introduction
Anatomical abnormalities
Degenerative conditions
Infections of the back and pelvis
Stress fractures
Neoplasia
Miscellaneous conditions of the vertebral bodies
References
16 Muscular Disorders of the Equine Back
Introduction
Diagnostic procedures
Disorders: aetiopathogenesis and treatment
References
17 Supraspinous Ligament and Dorsal Sacroiliac Ligament Desmitis
Introduction
Supraspinous ligament
Chronic and low-grade injuries
Dorsal sacroiliac ligament
Pathology of the DSIL
Lateral (long) portion of the DSIL
References
18 Sacroiliac Dysfunction
Anatomy
Incidence
Clinical signs
Diagnosis of SID
Management of SID
Conclusion
References
Section 4: Back Pathology in Specific Disciplines
19 Dressage Horses
Assessment of the dressage horse at exercise/competition
Common conditions
References
20 Showjumpers
The jumping effort
Diagnostic imaging
Specific back pathology in the showjumper
Treatment of the showjumper
References
21 Eventers
Introduction
Diagnostic approach
Treatment
Conclusions
Reference
22 Racehorses
Introduction
Most common diagnoses of back pathology in the racehorse
Approach to clinical cases
Main differential diagnoses for back pain in the thoroughbred racehorse
The role of diagnostic imaging in the detection of back pathology in the racehorse
Management problems leading to superficial injury
Treatment and management of back pathology in the racehorse
Reference
Section 5: Complementary Therapy and Rehabilitation
23 Complementary Therapies in the Treatment of Back Pain
Introduction
The horse’s body language
Difficulties in the clinical diagnosis of back pain
Communication and relaxation
Relaxation
Pain and performance
The role of the equine therapist
Therapies
Conclusion
References
24 Integrative Therapies in the Treatment of Back Pain
Introduction
Integrative approach to diagnosis of back pain
History of the horse with back pain
Observation of the horse
Palpation of the back
The use of diagnostic imaging
Saddle fit
Additional management factors influencing back pain
Treatments for back pain
Chiropractic and spinal manipulation
Ledum palustra (marsh tea)
Traumeel
Conclusion
References
Organisations and courses
25 Rehabilitation
Introduction
The back
Anatomy
Vertebral ligaments
Dorsal section
Ventral section
Back pain
Rehabilitation programmes
Rebuilding muscle
Why classical exercises?
Muscle loading
Early rehabilitation
Hydrotherapy – water as a rehabilitation aid
Conclusion
References
Supplemental images
Index
This edition first published 2009
© 2009 Blackwell Publishing Ltd
Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing programme has been merged with Wiley’s global Scientific, Technical, and Medical business to form Wiley-Blackwell.
Registered office
John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, United Kingdom
Editorial offices
9600 Garsington Road, Oxford, OX4 2DQ, United Kingdom
2121 State Avenue, Ames, Iowa 50014-8300, USA
For details of our global editorial offices, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell.
The right of the author to be identified as the author of this work has been asserted in accordance with the Copyright, Designs and Patents Act 1988.
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher.
Wiley also publishes its books in a variety of electronic formats. Some content that appears in print may not be available in electronic books.
Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their respective owners. The publisher is not associated with any product or vendor mentioned in this book. This publication is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold on the understanding that the publisher is not engaged in rendering professional services. If professional advice or other expert assistance is required, the services of a competent professional should be sought.
Library of Congress Cataloging-in-Publication Data
Equine back pathology : diagnosis and treatment / edited by Frances M.D. Henson.
p. ; cm.
Includes bibliographical references and index.
ISBN 978-1-4051-5492-5 (hardback : alk. paper) 1. Horses–Diseases–Diagnosis. 2. Horses–Diseases–Treatment. 3. Back–Diseases–Diagnosis. 4. Back–Diseases–Treatment. I. Henson, Frances M. D.
[DNLM: 1. Horse Diseases. 2. Back Pain–veterinary. 3. Spinal Diseases–pathology. 4. Spinal Diseases–veterinary. 5. Spine–anatomy & histology. SF 951 E631 2009]
SF951.E542 2009
636.1'089756–dc22
2008039843
A catalogue record for this book is available from the British Library.
1 2009
Contributors
David Bainbridge, VetMB MA PhD MRCVS
University Clinical Veterinary Anatomist
Department of Physiology, Development and Neuroscience, University of Cambridge,
Cambridge, UK
Andrew P. Bathe, MA, VetMB, DipECVS, DEO, MRCVS
RCVS and European Specialist in Equine Surgery
Rossdales Equine Hospital, Cotton End Road,
Exning, Newmarket, Suffolk, UK
Mary Bromiley, FRSP, SRP, RPT(USA)
Downs House Equine, Combeleigh Farm,
Wheddon Cross, Minehead, Somerset, UK
Adam Driver, BVSc, CertVR, MRCVS
Global Equine Group Ltd
9 The Manor, Herringswell, Bury St Edmunds, UK
Constanze Fintl, BVSc, MSc, PhD,
CertEM(IntMed), DipECEIM, MRCVS
Department of Companion Animal Clinical Sciences, Norwegian School of Veterinary
Science, Oslo, Norway
Joyce Harman, DVM, MRCVS
Harmany Equine Clinic Ltd, Flint Hill, Virginia, USA
Marcus J. Head, BVet.Med, MRCVS
Rossdale’s Diagnostic Centre, Cotton End Road,
Exning, Newmarket, Suffolk, UK
Frances M.D. Henson, MA, VetMB, PhD,
CertES(Orth), CertEM(Int Med), MRCVS
Queen’s Veterinary School Hospital, University of Cambridge, Cambridge, UK
Leo B. Jeffcott, MA, BVet.Med, PhD, FRCVS, DVSc, VetMedDr
Dean and Professor of Veterinary Science
Faculty of Veterinary Science, University of Sydney, JD Stewart Building, New South Wales,
Australia
Jessica A. Kidd, BA, DVM, CertES(Orth), Diplomate ECVS, MRCVS
The Valley Equine Hospital, Lambourn,
Berkshire, UK
Svend E. Kold, DrMedVet, PhD, CUEW, RFP, MRCVS
Willesley Equine Clinic Ltd, Byams Farm,
Willesley, Tetbury, Gloucestershire, UK
Luis P. Lamas, DVM CertES(Orth) MRCVS
Queen’s Veterinary School Hospital, University of Cambridge, Cambridge, UK
Graham A. Munroe, BVSc(Hons), PhD, CertEO, DESM, DipECVS, FRCVS
Flanders Veterinary Services, Cowrig Cottage,
Greenlaw, Duns, Berwickshire, UK
Alastair Nelson, MA, VetMB, CertVR, MRCVS,
Rainbow Equine Clinic, Old Malton, North
Yorkshire, UK
Richard J. Piercy, MA, VetMB, MS, PhD, DipACVIM, MRCVS
Comparative Neuromuscular Diseases Laboratory, Royal Veterinary College,
Hawkshead Lane, North Mymms, Hatfield, UK
Rob Pilsworth, BSc(Hons), MA, VetMB, CertVR, MRCVS
Newmarket Equine Hospital, Newmarket,
Suffolk, UK
Mimi Porter, MS
Equine Therapy Inc., 4350 Harrodsburg Road,
Lexington, Kentucky, USA
Tracy A. Turner, DVM, MS, DiplACVS, DiplABT
Anoka Equine Veterinary Services, Elk River,
Minnesota, USA
P. René van Weeren, DVM, PhD, DiplECVS
Professor of Equine Musculoskeletal Biology
Department of Equine Sciences, Faculty of Veterinary Medicine, Utrecht University, The Netherlands
Renate Weller, Drmedvet, PhD, MRVCS
Lecturer in Diagnostic Imaging
Department of Veterinary Clinical Sciences, The Royal Veterinary College, Hawkshead Lane,
North Mymms, Hatfield, UK
Mary Beth Whitcomb, DVM
Assistant Professor
Clinical Large Animal Ultrasound, Department of Surgical and Radiological Sciences, School of Veterinary Medicine, University of California,
Davis, California, USA
Foreword
In the fourth Sir Frederick Hobday Memorial Lecture that I delivered 30 years ago to the British Equine Veterinary Association, I ended with a quote from Mohammed. He wrote some 3000 years earlier “Care for your mares – their bellies are your treasure, their backs your safety, and God will help their owners”. For me this was proof indeed that the horse’s back is of considerable importance for their function and athletic ability.
At the time of the Hobday Lecture I highlighted six areas that I considered to be important limiting factors in the evaluation of back problems in the horse:
Much has happened in the intervening years and a great deal more interest has been paid to the horse’s back, both clinically and in research. This book serves to identify the considerable progress that has been made in addressing all these factors. So now it is possible to establish definitive diagnoses, to appreciate huge advances in our understanding of the biomechanics of the back, to evaluate the results of controlled studies on therapy and outcome, and to work really closely with our paraprofessional colleagues to better evaluate and treat horses with back problems. Despite these important advances there is still much work to be done. However, it is hoped that this book will help to maintain the interest in the horse’s back by informing interested people, teaching students, enthusing “old hands” who have been treating back cases for years and, most importantly, improving the diagnosis and management of all horses with back pathology.
Leo Jeffcott
Acknowledgements
This book would not have been written without the leadership, inspiration and support that Professor Leo Jeffcott has shown me throughout my career. Anything I know about the equine back comes from the foundations that he taught me.
I would also like to thank all of the horses that I have had the pleasure of examining and treating, the clinicians with whom I have worked for teaching me so much, all of the staff in the Equine Hospital, University of Cambridge (particularly Alison Smith and Graham Munroe), for supporting and humouring me, and all of the contributors to this book for putting up with my electronic nagging.
My grateful thanks to my mother and father, Joan and Mike, for giving me a love of horses and a scientific mind, and to my daughters, Claudia and Sofia, for being a delight and joy.
Special thanks, of course, to my wonderful husband, Mike, for simply everything.
Frances Henson
Abbreviations
| ACP | acepromazine |
| AP | articular process |
| AR | axial rotation |
| AF | articular facet |
| AMP | angular movement pattern |
| BHV | between-horse variability |
| C | cervical |
| CNS | central nervous system |
| Cy | coccygeal |
| DLVMO | dorsolateral–ventromedial–oblique |
| DMVLO | dorsomedial–ventrolateral–oblique |
| DSIL | dorsal sacroiliac ligament |
| DSP | dorsal spinous process |
| EEE | eastern equine encephalitis |
| EHV | equine herpesvirus |
| EPM | equine protozoal myeloencephalitis |
| FE | flexion–extension |
| GP | general proprioceptive |
| GSA | general somatic afferent |
| GVA | general visceral afferent |
| GSE | general somatic efferent |
| GVE | general somatic efferent |
| HNP | head and neck position |
| i.m. | intramuscularly |
| ISL | interspinous ligament |
| IT | intertransverse |
| L | lumbar |
| LB | lateral bending |
| LMN | lower motor neuron |
| NSAID | non-steroidal anti-inflammatory drug |
| OA | osteoarthritis |
| ORDSP | overriding dorsal spinous processes |
| p.o. | per os |
| PNS | peripheral nervous system |
| ROI | region of interest |
| ROM | range of motion |
| S | sacral |
| SID | sacroiliac dysfunction |
| SIJ | sacroiliac joint |
| SIL | sacroiliac ligament |
| SSL | supraspinous ligament |
| SWL | shock wave therapy |
| T | thoracic |
| TB | thoroughbred |
| TP | transverse process |
| UMN | upper motor neuron |
| VSL | ventral sacroiliac ligament |
| WEE | western equine encephalitis |
| WHV | within-horse variability |
In order to understand the pathological conditions that affect a horse’s back it is necessary to have an excellent working knowledge of its structure. The back and pelvis are made up of osseous structures, joints, muscles, ligaments, blood vessels and nerves, all of which can be altered or affected in disease. In this chapter the osseous structures of the back (i.e. the thoracolumbar spine, sacrum and pelvis) are discussed. The soft tissues (i.e. muscles and ligaments) and the innervation of the back are dealt with in Chapters 2, 3 and 4 respectively.
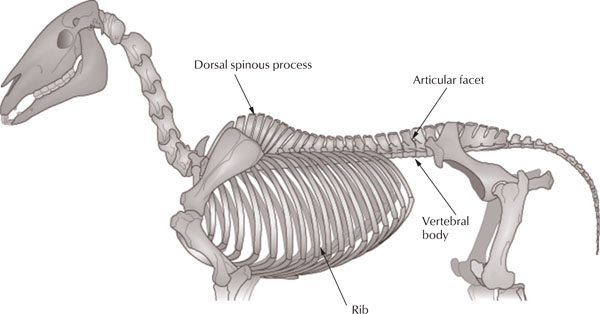
The vertebral column runs from the atlanto-occipital joint to the last coccygeal vertebra (Figure 1.1). As it passes through the body the vertebral column does not form a straight-line structure; rather it descends sharply from the atlanto-occipital joint to reach its lowest point at the cervicothoracic junction. The column then ascends gently to the caudal lumbar region and descends down, via the sacrum, to the coccygeal vertebrae (Figure 1.1). The external appearance of the horse, however, presents a different picture in the cranial thoracic region. Externally the withers (corresponding approximately to T3–7) is the highest point of the back, even though the vertebral bodies are ventral to most other vertebral bodies at this point. This is due to the external elevation provided by the long dorsal spinous processes (DSPs) in the withers region, which creates a contrary impression [1].
The nomenclature for the classification of different vertebral segments is fairly standardised between different texts and papers, with vertebral segments traditionally counted within spinal regions from a cranial reference point. Within each region the vertebrae are numbered sequentially from cranial to caudal, e.g. T1 (first thoracic vertebra), T2 (second thoracic vertebra). However, occasionally, some authors use modified reference systems, using caudal reference points [2]. It is important to be aware of this alternative numbering system when consulting the literature in this area to avoid confusion. In this book the standard cranial reference system will be used.
The spine of the horse is made up of cervical, thoracic, lumbar, sacral and coccygeal vertebrae (Figure 1.2). The standard vertebral formula for the horse is 7 cervical vertebrae, 18 thoracic vertebrae, 6 lumbar vertebrae, 5 sacral vertebrae and between 15 and 21 coccygeal vertebrae [3] (Table 1.1).
Figure 1.1 A photograph of the skeleton of the horse. The vertebral column runs from the atlanto-occipital joint to the last coccygeal vertebra. The vertebral column descends sharply from the atlanto-occipital joint to reach its lowest point at the cervicothoracic junction. The column then ascends gently to the caudal lumbar region and descends down, via the sacrum, to the coccygeal vertebrae.
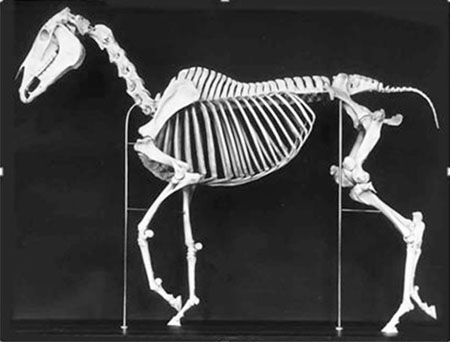
Figure 1.2 The bones of the vertebral column from the seventh cervical vertebra to the penultimate coccygeal vertebra. The vertebral column is divided into cervical, thoracic, lumbar, sacral and coccygeal regions. There are 7 cervical vertebrae, 18 thoracic vertebrae, 6 lumbar vertebrae, 5 sacral vertebrae and 15–21 coccygeal vertebrae in the normal horse.
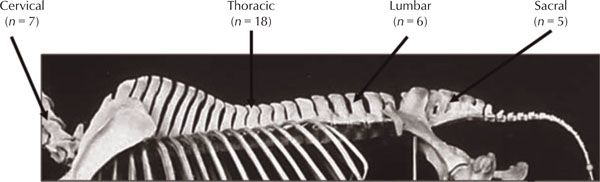
Table 1.1 Average vertebral formula for the horse
| Anatomical site | Number of vertebrae |
| Cervical | 7 |
| Thoracic | 18 |
| Lumbar | 6 |
| Sacral | 5 |
| Coccygeal | 15–21 |
Although there may be some variation in the number of specific vertebrae in the axial skeleton, the total number in the formula is more constant. Anecdotally, so-called “short-backed” horses, such as Arabians, have been reported as having fewer vertebrae than other horses [4]. More objective data on the numbers of vertebrae have come from studies investigating the numbers of vertebrae within a population, with a number of studies designed to investigate the frequency of occurrence of the standard six lumbar vertebrae. Haussler et al. [2], in a study on thoroughbred horses, showed that only 69% of horses had the expected six lumbar vertebrae. However, it has been suggested that variations in the number of vertebrae within one spinal region are compensated for by an alteration in number in an adjacent vertebral region, in many cases to give a constant overall total vertebral number. There has been no proven association between the numbers of vertebrae that a horse has and any pathological condition.
Before a description of the different anatomical features of vertebrae at different anatomical sites in the vertebral column, “transitional vertebrae” must be considered. Transitional vertebrae are located between two adjacent vertebral regions and have the morphological characteristics of both these regions, i.e. they are “hybrid” vertebrae. They occur, therefore at the cervicothoracic, thoracolumbar or lumbosacral junction. A few studies have documented the incidence of transitional vertebrae. Haussler et al. [2] showed that 22% of their study population had thoracolumbar transitional vertebrae, none had lumbosacral transitional vertebrae and 36% had sacrococcygeal transitional vertebrae. Transitional vertebrae may exhibit their unusual morphology either through left-to-right asymmetry or via altered cranial-to-caudal graduation in the morphology. In large-scale studies of lumbosacral transitional vertebrae in humans and dogs, the morphological characteristics of the transitional vertebrae have been demonstrated to occur at the vertebral arches and transverse processes rather than at the vertebral body.
In clinical practice the most common transitional vertebra is transitional C7, which is often detected on lateromedial radiographs of the base of the spine and is characterised by having a short DSP, when it would normally have none at all.
The primary ossification centres of the vertebral bodies and neural arches (i.e. those surrounding the embryonic notochord in the centrum and lateral to the neural tube in the vertebral arch) fuse shortly after birth [5], whereas the secondary separate centres of ossification do not fuse until later on in life, if at all.
Secondary centres of ossification occur in the summits of the DSPs of the cranial thoracic vertebrae (the caudal thoracic and lumbar DSPs have fibrocartilaginous caps), the extremities of the transverse processes (TPs) of the lumbar vertebrae, the epiphyses of the vertebral bodies and the ventral crest.
The age at which these secondary centres of ossification fuse to the parent bone depends on the method of estimation of growth plate closure. Postmortem and histological growth plate closure times will always report an older age of closure than radiographic surveys because radiography is a less sensitive method of identifying the presence of an open growth plate.
The secondary centres of ossification present in the summits of the DSPs of the cranial thoracic region from T2 to around T9 are reported to fuse to the parent bone between 9 and 14 years of age [3], but in many cases, in the author’s experience, they never fuse to the parent bone, even in aged horses. Thus they can be confused with fractured summits of the DSPs on radiographs if this developmental feature is not appreciated (see Figure 8.6 in Chapter 8).
The secondary centres of ossification at the cranial and caudal epiphyses of the vertebral bodies have reported closure times of between 3 and 3½ years of age using radiographic techniques (see Figure 8.4 in Chapter 8) [5]. However, gross anatomical studies suggest that the plates fully close later and asynchronously. The physes are reported to close between 4.9 and 6.7 years, with the cranial physis closing first, usually 1–2 years before the caudal physis [2].
The secondary centres of ossification of the TPs close in the first few months of life, although specific reports of this are not available.
A typical thoracic vertebra is made up of a vertebral body, a vertebral arch and vertebral processes (Figure 1.3). The vertebral body provides the surface against which the intervertebral disc sits, whereas the vertebral arch provides a gap in the osseous structure through which the spinal cord runs. The vertebral processes are the sites of attachment for various ligaments and muscles and are named the dorsal spinous processes, the transverse processes and the articular processes (APs) (Figure 1.3). These processes vary subtly within each anatomical region and this variation reflects the functional and structural demands at that particular anatomical site, e.g. the length of the DSP varies from region to region, being particularly long between T3 and T7. The lumbar vertebrae, in contrast, have long TPs and medium height DSPs.
The vertebral bodies of the equine thoracolumbar spine (see Figure 1.4) provide support for weight-bearing and attachment sites for soft tissues and muscles. They are convex in shape cranially and concave in shape caudally. Ventrally a ridge of bone, the “ventral crest” (see Figure 1.3) is observed on approximately four to eight vertebrae (mean 5.5 ± 0.8 [2]) centred around the thoracolumbar junction.
The shape of the vertebral bodies changes from a rounded shape in the thoracic region to a dorsoventrally flattened shape in the caudal lumbar and sacral regions. It has been hypothesised that this shape change limits movement laterally between these vertebrae, but not dorsoventrally. Other anatomical variations between sites include the observation that prominent ventral body ventral crests are found in the cranial thoracic area and between T15 and L3. The ventral crest at the latter site, which can vary in the number of vertebrae involved, is believed to be the site of insertion of the crura of the diaphragm.
Figure 1.3 Vertebral anatomy: (a, b) line diagrams of a thoracic vertebra labelled to show the different anatomical regions of the vertebra: (a) a craniocaudal oblique diagram, (b) a lateral diagram. (c, d) Photographs of typical vertebrae: (c) thoracic vertebra, (d) lumbar vertebra; A, vertebral body; B, vertebral canal; C, dorsal spinous process; D, articular facet; E, transverse process. Note the much longer transverse processes in the lumbar vertebra compared with the thoracic vertebra.
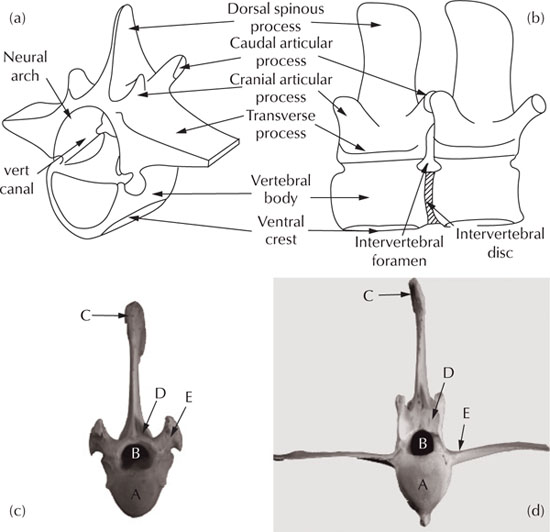
Figure 1.4 A line drawing of the skeleton showing the relative positions of the dorsal spinous processes, articular facets, vertebral bodies and ribs.
The intervertebral discs (or fibrocartilages) are positioned between adjacent vertebral bodies and, together, they are correctly described as fibrocartilaginous articulations. They function to aid weight bearing, axial shock absorption and the maintenance of vertebral flexibility; they have both proprioceptive and nocioceptive fibres in the outer third of the disc. The discs are made up of a gelatinous central nucleus pulposus and an outer fibrous annulus fibrosus; this annulus fibrosus is designed to provide rotational stability to the intervertebral joint by being formed of concentric layers of fibres angled relative to each other.
The width of the intervertebral discs differs between anatomical sites. In one study it was demonstrated that the intervertebral discs were thicker at T1–2 (average 5.9 mm, [6]) than elsewhere in the thoracic spine, with the average diameter of an intervertebral disc in the midthoracic region being 2.5 mm. It was also shown that the lumbosacral junction has a wider intervertebral disc compared with elsewhere in the spine (average 3.6 mm).
In the horse, relatively few clinical problems arise from intervertebral disc pathology, particularly compared with the high frequency of pathology at this site in dogs and humans. However, discospondylitis and intervertebral disc degeneration are occasionally seen (see Chapter 15). Intervertebral disc herniation is extremely rare in the horse, possibly because of the poorly developed nucleus pulposus and thin intervertebral disc.
The spinal cord runs through the vertebral arch, which is made up of the dorsal part of the vertebral body ventrally, the vertebral lamina dorsally and the pedicles laterally. Dorsally in the vertebral arch the ventral laminae are connected by the ligamenta flava. The vertebral arches of the spinal vertebrae together form the continuous vertebral canal housing the spinal cord and its associated structures up to the cranial sacral region where the spinal cord terminates in the cauda equina (see Chapter 4). The vertebral arch is relatively large compared with the diameter of the spinal cord, ensuring no compression of the cord during movements of the spinal segments in the normal spine. However, in pathological conditions narrowing of the vertebral arch can occur (i.e. if there is displaced bone secondary to a fracture or new bone formation in osteoarthritis). In these cases spinal cord compression may result in onset of neurological signs.
Figure 1.5 Intervertebral and lateral foramina of the thoracic spine: (a, c) photographs of a skeleton; (b) a cross-section from a postmortem specimen; (d) a lateromedial radiograph. In (a) an open intervertebral foramen is seen (black arrow) in the vertebral segment cranial to an intervertebral foramen that has spurs of bone formation protruding into it from dorsal and ventral (arrow head). In (b) this new bone formation is seen on the postmortem specimen. In (c) a strut of new bone is seen bridging the intervertebral foramen to form a lateral foramen. In (d) an open intervertebral foramen is seen cranial to two lateral foramina (circular radiolucencies).
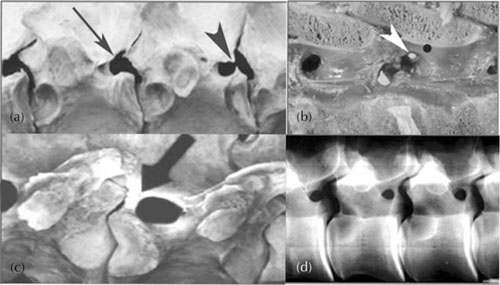
Between the vertebral arches of each vertebra there is a small opening on either side – the inter-vertebral foramina (Figure 1.5a). These intervertebral foramina are formed by ventral notches in the cranial and caudal margins of the vertebral arch. The intervertebral foramina permit soft tissue structures (nerves, blood vessels and lymphatics) to exit the bony vertebral canal at each segment.
In addition to the intervertebral foramina that are observed on either side of the spine at each segmental junction between vertebrae, a second lateralised opening out of the bony canal is also present intermittently in some individuals. These are known as the lateral foramina (Figure 1.5c and d). Thoracic vertebrae T11, T15 and T16 have been reported as showing the highest incidence of fully formed lateral foramina in the thoracolumbar spine [7].
The origin of the lateral foramina is not known; however, it has been proposed that they arise from the intervertebral foramina as a consequence of spur formation in the caudal ventral notch of the vertebral arch (Figure 1.5a). Progressive calcification of the caudal ventral notch can occur, similar to that seen in ventral spondylitis (Figure 1.5c) (see Chapter 15). In addition to a fully enclosed lateral foramen, there are a number of other variations in the anatomy of the caudal notch of the vertebral arch, including one or more spurs protruding into the notch [7]. It has been demonstrated that, where present, the lateral foramen contains spinal nerves and some vessels, and the presence of lateral foramina may possibly be associated with spinal nerve impingement during and subsequent to this calcification.
In the sacrum the soft tissue structures exit the fused vertebral arches via either dorsal or ventral (pelvic) sacral foramina. The dorsal branches of the sacral spinal nerves exit via the dorsal sacral foramina. The pelvic sacral foramina communicate with the vertebral canal ventrally and contain the ventral branches of the sacral spinal nerves.
The vertebral canal contains the spinal cord and the structures surrounding the spinal cord (i.e. the cerebrospinal fluid, meninges, fat and vascular plexus). The spinal cord has segmentally paired dorsal and ventral motor roots that converge within the intervertebral foramen to form the spinal nerves (see Chapter 4).
The DSPs project dorsally from the vertebral arch to rise above the vertebra into the epaxial musculature. The function of the DSPs is considered to be as levers for the muscular and ligamentous attachments of the vertebral column; bilateral contraction of the muscles that attach to the DSPs causes spinal extension, and unilateral contraction causes rotation.
The DSPs vary in their length, shape and angulation in different regions and will be considered anatomically from T1 running caudally. T1 has an extremely small DSP, rising approximately to twice the height of the vertebral body dorsally (Figure 1.6). This is the first elongated DSP in the vertebral column in most horses; however, occasionally an elongated DSP is seen on C7 (i.e. C7 has the properties of a transitional vertebra). Care must be taken not to automatically assume that the first obvious DSP on a lateromedial radiograph is therefore T1.
Although T1 has a small spinous process, the DSPs in the cranial thoracic vertebral region are markedly elongated in the region of T2–8 to form the withers (Figure 1.7). The apex of the withers is formed by the DSPs of T4–7 (Figure 1.7a). As noted above the tips of the DSP of approximately T4–7 have separate centres of ossification. From an apex at T6 or T7 the length of the DSP decreases down to approximately T12; the height of the DSP decreases slightly down to the anticlinal vertebra (the vertebra at which the angulation of the DSPs changes, see below; Figure 1.7b) and then increases gently to the last lumbar vertebra (Figure 1.7c).
The shape of the DSPs also depends on the anatomical site from which they arise. DSPs from vertebrae T1–10 are narrow and tend to be quite straight (Figure 1.7a). At T11–16 they have a marked beak-shaped outline, wider at their base than at their apex and forming a cranial beak with a rounded caudal aspect at their summits. The cranial and caudal borders of the DSPs are often roughened due to new bone formation on these edges, which are the insertions of the interspinous ligaments; the dorsal summits of the DSPs are also often roughened at the sites of attachment of the supraspinous ligament (see Chapter 10).
Figure 1.6 A photograph of vertebrae cervical 7 (C7) and thoracic 1 (T1). Note the elongated dorsal spinous process on T1 (arrow) compared with C7 (arrow head).

Figure 1.7 Three photographs of the vertebral column of a horse showing the shape and angulation of the dorsal spinous processes (DSPs): (a) cranial thoracic region (withers); the DSPs are markedly elongated and angle caudally. Note the separate centres of ossification in the most cranial vertebrae. In (b) the DSPs of the mid-thoracic region are seen. At this site the DSPs are shorter than in the cranial thoracic region and have a ‘beak shape’ at their summits. The DSPs of the more cranial vertebrae angle caudally until the ‘anticlinal’ vertebra (black arrow). From this point caudally the DSPs angle cranially. In (c) the DSPs of the caudal thoracic and first four lumbar vertebrae are seen. The DSPs angle cranially.
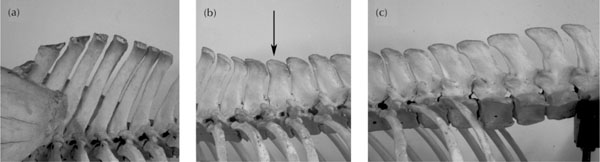
The angulation of the thoracolumbar DSPs changes from T1 caudally to the lumbosacral junction. From T1 to T14 the DSPs are angled dorsocaudally (i.e. towards the tail; Figure 1.7a). At T15, the so-called “anticlinal vertebra” (Figure 1.7b), the DSP is upright and then from T17 to L6 the DSPs are angled dorsocranially (towards the head) (Figure 1.7c). The anatomical reason for this alteration in DSP angulation is suggested to be due to attached soft tissue interactions. The position of the anticlinal vertebra suggests an alteration, at this anatomical site, of the soft tissue forces acting on the spine. The cranial thoracic region transmits forces from the head, neck and forelimbs, whereas the caudal thoracic and lumbosacral regions transmit forces associated with the hindlimbs; therefore the pull of the associated soft tissue structures does indeed alter either side of the anticlinal vertebra.
A further change in DSP angulation is observed in the sacrum, which is inclined dorsocaudally (Figure 1.8). The anatomical consequence of this alteration in angulation, without the intermediary of an anticlinal vertebra as occurs in the thoracic spine, is that a wide interspinous space is formed at the lumbosacral junction (Figure 1.8). It has been suggested that this wide interspinous space allows an increased range of motion at this site without the risk of process impingement. The wide space between L6 and S1 is a relatively consistent finding; however, in one study 36% of horses had an equally wide interspinous space between L5 and L6 [2]. This has, at the current time, little clinical relevance apart from possibly making more difficult the identification of the landmarks for cerebrospinal fluid retrieval from the lumbosacral space.
Figure 1.8 A photograph of the lumbosacral region: the wing of the ilium is seen in front of the cranial part of the sacrum. The last lumbar vertebra angles cranially and the sacrum angles caudally. The lumbosacral space is wide compared with any other interspinal space in the vertebral column (black arrow).

The distance between the summits of the DSPs varies between anatomical sites and between individuals. In most horses there is a small but clear gap between the DSP in the region T1 to T11; however, after T11 the DSPs become closer together. In some cases, post mortem or on lateromedial radiographs, the DSPs are seen to overlap with no evidence of bony contact (i.e. they are not quite in the same sagittal plane). Thus there is no bony contact and no evidence of bony remodelling. However, in many cases the close proximity of the DSPs does lead to bony contact, remodelling and, in some cases, false joint formation. This condition is known variously as “kissing spines” or “overriding dorsal spinous processes” and can cause back pain (see Chapter 14).
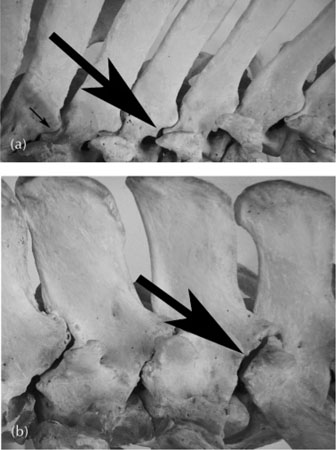
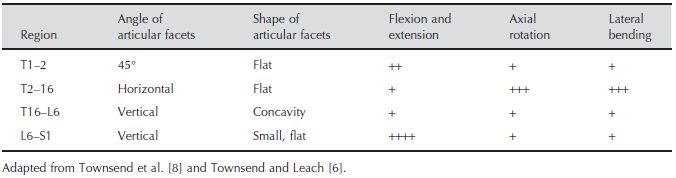
Paired articular processes (facets) arise both cranially and caudally from the vertebral arch and extend dorsally laterally. Between the cranial articular process of one vertebra and the caudal articular process of an adjacent vertebra a synovial joint is formed (i.e. a zygapophyseal joint). At each vertebral junction a pair of these joints is thus formed. The size, shape and orientation of the articular facets and hence joint surface differ within the vertebral column. In the cervical region and T1 the articular surfaces are large and lie at 45° to the horizontal. At T2 there is a transition from a 45° angle to a horizontal positioning of the articular facets. In the remainder of the thoracic region until about T16 (in 11 of 21 horses [6]), the articular surfaces continue to lie approximately horizontal with the cranial articular surfaces facing dorsally and the caudal articular surfaces facing ventrally (Figure 1.9a). The morphology of the articular facets is, however, not always symmetrical; one study reported that 83% of horses had asymmetrical facets [2]. At T16 and then into the lumbar region the articular surface orientation changes from horizontal to vertical (Figure 1.9b). In addition to the change in orientation of the articular facets, changes are also seen in the actual shape of the processes. In the thoracic region the facets are relatively flat; from T16 onwards their articular surfaces change such that the cranial articular surfaces are dorsally concave and the caudal articular surfaces ventrally convex. The alteration in the angulation and shape of the articular processes may reflect the movements of the different parts of the spine; in the thoracic vertebral region vertebral motion is mostly rotation and lateral flexion. In the lumbosacral region motion is mainly dorsoventral.
Figure 1.9 Two photographs to show the angulation of the articular facets at different regions of the vertebral column: (a) cranial thoracic vertebrae; articulations are close to horizontal (black arrows). (b) Caudal thoracic vertebrae: articulations are more vertically oriented (black arrow).
It has been proposed, based on the morphology of the articular facets, that the equine thoracolumbar spine can be divided into four regions: the first thoracic intervertebral joint (T1–2), the cranial and mid-thoracic region (T2–16), the caudal thoracic and lumbar region (T16–L6), and the lumbosacral joint (L6–S1) [6]. Studies on the amount and type of movement at each of these sites have indicated that each of these four sites does have a characteristic movement [8] and thus a structure–function relationship at these sites is likely (Table 1.2).
The TPs exit the vertebrae at right angles to the direction of travel of the spinal cord and protrude out into the soft tissues of the back. Their function seems to be as lever arms to provide support to the vertebral column, and permit movement of the column via the muscles and ligaments that attach to them. Thus the TPs serve to maintain posture and permit rotation and lateral flexion. TPs alter in length at different sites within the vertebral column. In the cranial thoracic vertebral region the TPs are short and blunt in the thoracic region. In the lumbar region the TPs are markedly elongated and flattened horizontally (see Figs 1.3 and 10.4 in Chapter 10). These TPs provide attachment sites for a number of muscles, including iliopsoas.
Table 1.2 The relative amounts of movement in the joint complexes of the four regions of the equine thoracolumbar spine and the structure of the articular facets at each site
The TPs have articulations with a number of different osseous structures, again dependent on site. In the thoracic region the TPs articulate with the ribs at the costotransverse articulations. In the lumbar region the horse is unusual in that there are intertransverse synovial articulations between the TPs of the last two or three lumbar vertebrae and the lumbosacral articulation [6, 9]. The latter articulation has the largest surface area, with more cranial articulations being smaller. These inter-transverse articulations usually occur as paired structures at any given anatomical site; however, asymmetrical distributions of these articulations have been reported (9% [9] and 14% [2]). The number is not constant between horses and it has been suggested that the number of lumbar vertebrae dictates the numbers of intertransverse articulations (i.e. horses with six lumbar vertebrae have an extra articulation [10]). The genus Equus and the rhinoceroses are the only mammals with this particular anatomical feature.
In addition to intertransverse articulations found in all horses, intertransverse ankylosis has also been a relatively common finding [6, 11], with Smythe [12] reporting its occurrence in 50% of horses. The relationship between intertransverse ankylosis and back pain has not been proved in the horse.
The lumbosacral junction is the articulation between the last lumbar vertebra and the sacrum (see Figure 1.8). As discussed above, in most individuals, the DSPs of the lumbar vertebrae point cranially, whereas the sacral DSPs point caudally, giving an ‘open’ lumbosacral space (i.e. a large gap between DSPs dorsal to the bony roof of the vertebral arch). In some cases a large open inter-spinous space is also noted between L5 and L6.
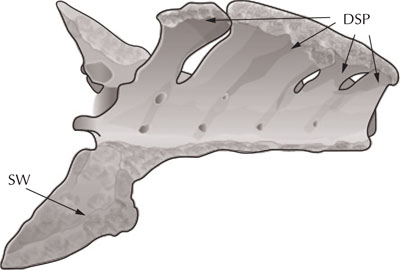
The sacrum of the horse is a triangular structure with slightly convex dorsal and concave ventral surfaces. In most horses it is made up of five vertebrae that become fused by the age of 5 years (Figure 1.10 and see Figure 1.8). The sacral vertebrae have two secondary centres of ossification, which can be visualised radiographically after birth: the cranial and caudal sacral internal physes. The cranial physis closes at 5.4 ± 1.5 years, the caudal one at 5.0 ± 1.5 years [2].
In the sacrum the spinal cord passes through the vertebral canal, which is formed from the fused vertebral arches. The spinal nerves exit the sacrum via dorsal and ventral sacral foramina – the sacral version of the thoracic and lumbar intervertebral foramina as discussed above. The sacral spinal nerves and the lumbar spinal nerves form the lumbosacral plexus.
The vertebral column articulates with the pelvis at the bilateral sacroiliac joints (see Chapter 18). It is at this site that the propulsive forces of the hindlimb are transferred to the vertebral column. The sacroiliac joint is actually a highly specialised point of contact, essentially between two flat bony surfaces. The point of contact is a synovial joint with unusual histological characteristics. Most synovial joints in the body are formed between two hyaline cartilage surfaces; in the sacroiliac region the joint is formed between a hyaline cartilage surface (sacral surface) and a fibrocartilage surface (ilial surface) [13].
Unlike other important synovial joints in the body the sacroiliac joint does not have the advantage of osseous contouring to aid the maintenance of joint integrity, as is found, for example, in ball-and-socket joints. Therefore, in order to provide biomechanical stability to the meeting of two flat surfaces, the horse uses three strong sacroiliac ligaments: the dorsal sacroiliac, ventral sacroiliac and interosseous sacral ligaments. These ligaments are discussed in detail in Chapter 3.
Figure 1.10 Line diagram of the sacrum: DSP, dorsal spinous processes of sacral vertebrae; SW, sacral wing.
Haussler [10] points out that an often overlooked aspect of the vertebral column is the large number of articulations present. He considered that the vertebral column was unique because of the potential for the presence of two types of articulation at each vertebral segment: a synovial articulation between the articular processes and a fibrocartilaginous articulation at the intervertebral disc. The exact number of articulations at each anatomical site varies (Table 1.3).
The bony pelvis of the horse is made up of the os coxae, the sacrum and the first two or three coccygeal vertebrae. The os coxae has three parts – the ilium (os ilii), the ischium (os ischii) and the pubis (os pubis) – which meet at the acetabulum (i.e. the cavity into which the head of the femur fits and articulates) (see Figure 1.11). The three parts of the os coxae are present in the developing fetus but become fused by 1 year of age. The growth plate closure times of the pelvis are detailed in Table 1.4.
Figure 1.11 Line diagrams of the dorsal and ventral surfaces of the pelvis to demonstrate the anatomy: (a) dorsal pelvis; (b) ventral view. TC, tuber coxae; TS, tuber sacrale; TI, tuber ischii; IS, ilial shaft; IW, ilial wing; P, pubic symphysis.
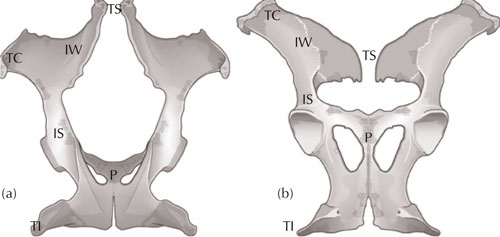
Table 1.3 The number of articulations at different anatomical regions of the spine
| Anatomical site | No. of articulations | Articular surfaces |
| Thoracic vertebrae | 12 | 2 intervertebral discs |
| 4 synovial intervertebral | ||
| 4 costovertebral | ||
| 2 costotransverse | ||
| Cranial lumbar vertebrae | 6 | 2 intervertebral discs |
| 4 synovial intervertebral | ||
| Caudal lumbar vertebrae | 10 | 2 intervertebral discs |
| 4 synovial intervertebral | ||
| 4 synovial intertransverse processes | ||
| Sacral vertebrae | 0 | Fused; no articulations |
Table 1.4 The growth plate closure times of the equine pelvis
| Anatomical site | Growth plate closure time (years) |
| Tuber sacrale | 5.8 ± 1.2 |
| Tuber coxae | 5.8 ± 1.5 |
| Ischial tuberosity | 5.2 ± 1.4 |
| Pubic symphysis | 5.7 ± 1.4 |
The ilium, the largest of the three bones. can be subdivided into different structural and functional areas (see Figure 1.11). The largest and widest part of the bone is the ilial wing, the most dorsal part of the ilium is the tuber sacrale, the most ventral and lateral part of the ilium is the tuber coxae, and the most medial part is the ischiatic spine.
The ilial wing itself has two surfaces: the gluteal (outer) and the pelvic (inner) surfaces. The surface of the ilium has a number of modifications of structural importance. The gluteal line is found running from the tuber coxae to the middle of the medial border. The middle and deep gluteal muscles attach here. The ilium is also modified to allow the passage of important vessels and nerves to cross its surface. The iliolumbar artery crosses the lateral border of the ilium, the iliacofemoral artery also crosses the lateral border more ventrally, just above the psoas tubercle (site of attachment of psoas minor), and the sciatic nerve runs over the medial surface of the bone at the greater sciatic notch.
The tuber sacrale is the highest point of the skeleton in most horses. At this point the ilial wing curves upwards and caudally and, at the summit, the tuber sacrale is roughened to provide the attachment for the dorsal sacroiliac ligament.
The tuber coxae is the most lateral part of the pelvis and forms the “point of the hip”. The tuber coxae is the elongated lateral angle of the pelvis, narrow in the middle of the angle and enlarged at either end.