7
Chapter 3 Inflammation, tissue repair and regeneration
Inflammation
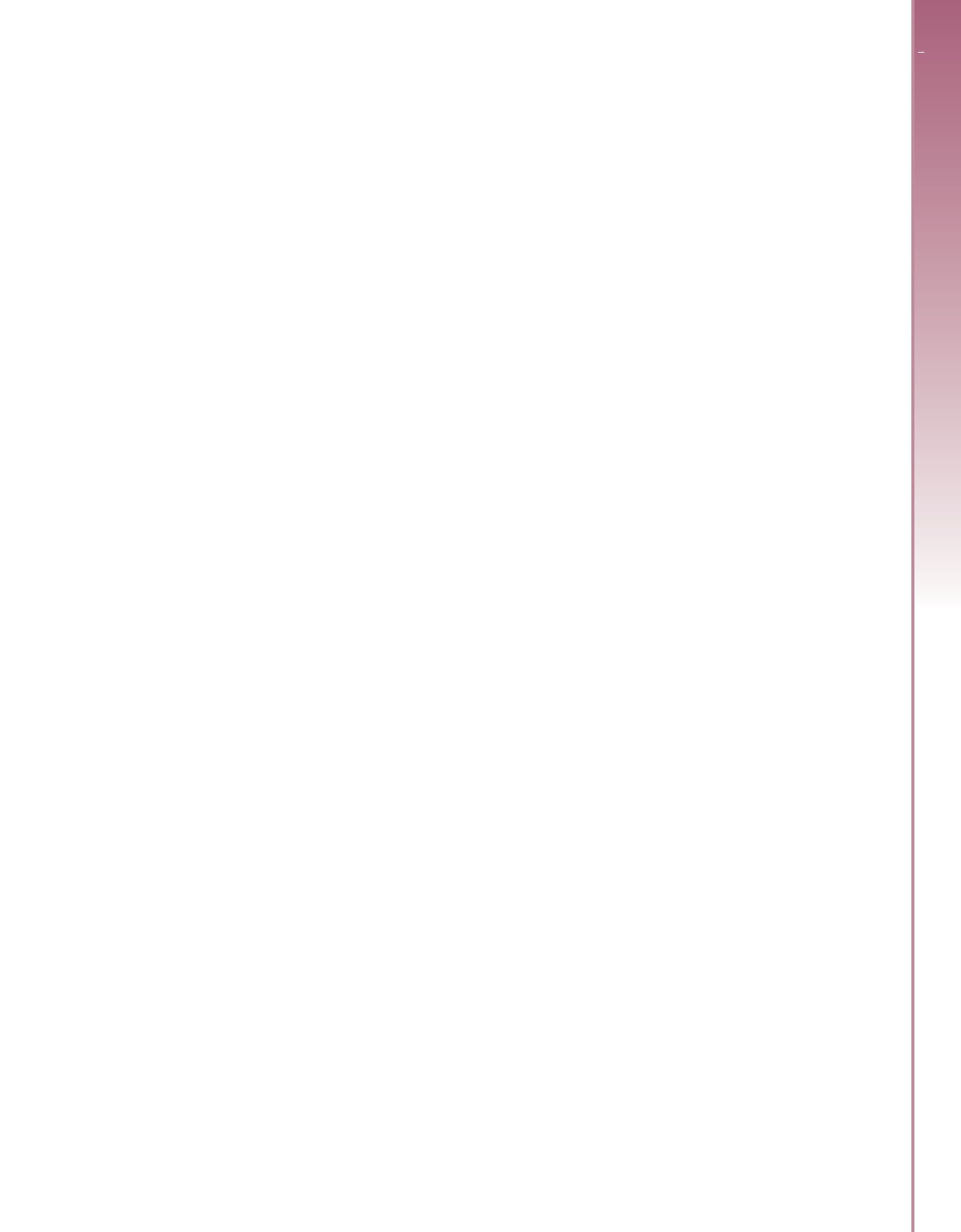
Inflammation is the body’s attempt at self protection; the
aim being to remove harmful stimuli, including damaged cells,
irritants or pathogens, and begin the healing process. Inflammation
can be defined clinically as the presence of swelling, redness and
pain. Some diseases associated with inflammation include arthri-
tis and neurological diseases. The signs and symptoms of inflam-
mation are caused by four processes: (1) mast cell degranulation,
(2) activation of plasma proteins, (3) the immune response and
(4) heat. All these processes occur simultaneously to produce
what is known as the inflammatory response. First, mast cell
degranulation, is the release of granules containing serotonin and
histamine from the mast cells into the tissues. These work with the
other two processes below to provide the complete inflammatory
signs and symptoms.
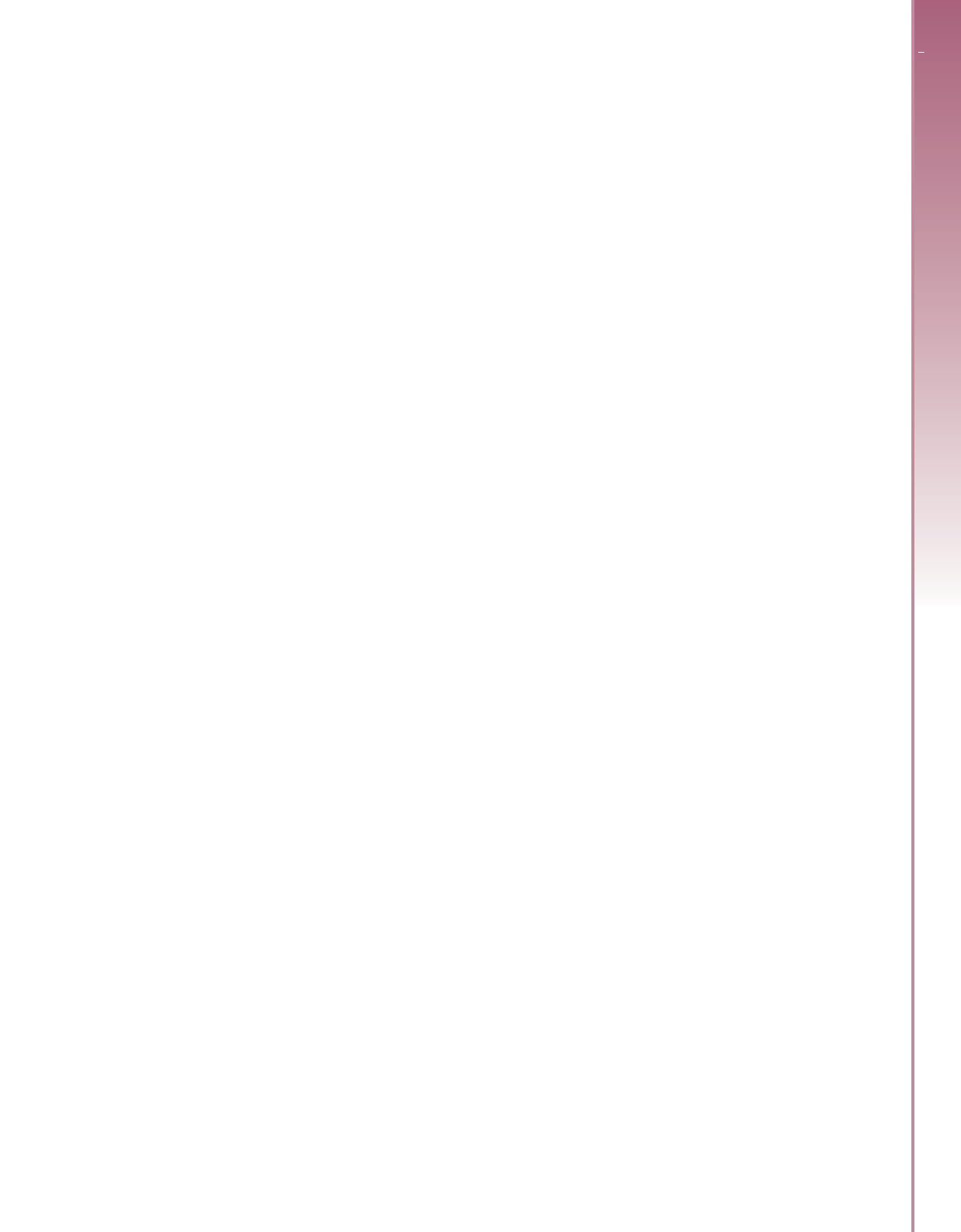
The second process involves the activation of four plasma pro-
tein systems: complement (helps to orchestrate the inflammatory
response); clotting (stops bleeding and repairs damage); kinin
(involved in vascular permeability); and immunoglobulins
(destroy bacteria), all of which work together to support the
inflammatory process. This activates and assists inflammatory and
immune processes, and also plays a major role in the destruction of
bacteria. The third process is the movement of phagocytic cells to
the area in order to phagocytose bacteria or any other non self
debris in the wound (Figure 3.2). The fourth process, heat, is a pro-
tective attempt by the organism to remove the injurious stimuli
and initiate the healing process. Without this heating, wounds
would never heal.
Physical and mechanical barriers
These are part of the first line defence against microorganisms.
They include the skin and the epithelial cells of the viscera, geni-
tourinary and respiratory tracts. The epithelial cells produce
mucus to protect the lining of the tracts, some contain cilia to
move the pathogens out and the temperature of the skin inhibits
microorganisms from colonizing on the skin.
Biochemical barriers
Epithelial surfaces also provide both physical and biochemical bar-
riers against infection. Some of these substances include sweat,
saliva, which contains enzymes to destroy bacteria, and tears.
Perspiration makes the skin pH slightly acidic, which is not a good
environment for the bacteria to grow.
Acute and chronic inflammation
Acute inflammation starts rapidly (rapid onset) and quickly
becomes severe. Signs and symptoms are only present for a few
days, but in some cases may persist for a few weeks. Some exam-
ples include acute bronchitis, appendicitis and sore throat
Chronic inflammation means long term inflammation, which
can last for several months and even years. Some examples include
chronic asthma, chronic peptic ulcer and chronic sinusitis.
Tissue repair
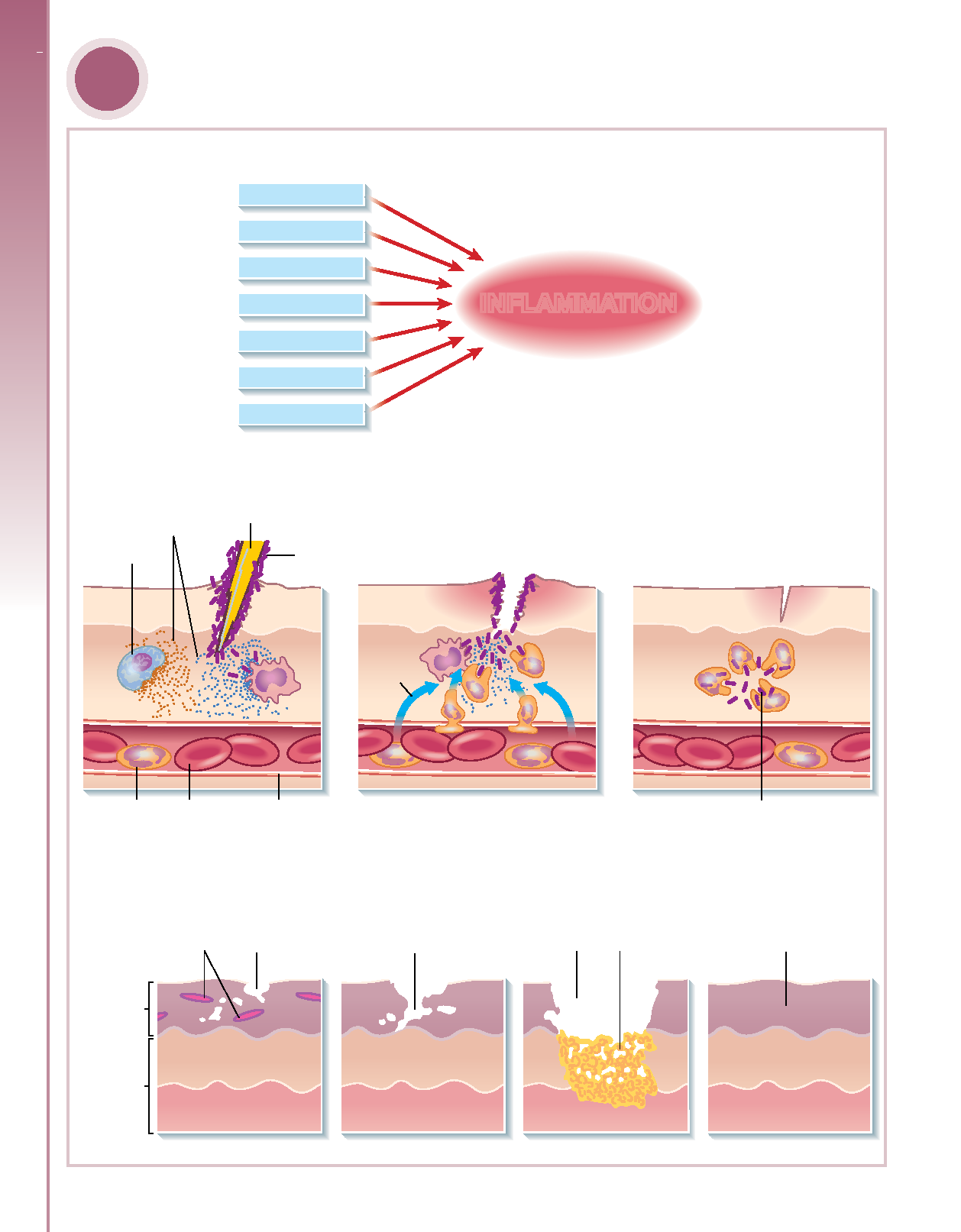
Wound healing, or cicatrization, is an intricate process in which
the skin (or another organ tissue) repairs itself after injury. In
normal skin, the epidermis (outermost layer) and dermis (inner
or deeper layer) exists in a steady state equilibrium, forming a
protective barrier against the external environment. Once the
protective barrier is broken, the normal (physiological) process of
wound healing is immediately set in motion. The classic model of
wound healing is divided into three or four sequential, yet
overlapping, phases: (1) haemostasis (not considered a phase by
some), (2) inflammatory, (3) proliferative and (4) remodelling.
Upon injury to the skin, a set of complex biochemical events take
place in a closely orchestrated cascade to repair the damage.
Within minutes post injury, platelets (thrombocytes) aggregate at
the injury site to form a fibrin clot. This clot acts to control active
bleeding (haemostasis). The speed of wound healing can be
impacted by many factors, including the bloodstream levels of
hormones such as oxytocin.
In the inflammatory phase, bacteria and debris are phagocytosed
and removed, and factors are released that cause the migration and
division of cells involved in the proliferative phase.
The proliferative phase is characterized by angiogenesis,
collagen deposition, granulation tissue formation, epithelializa-
tion, and wound contraction. In angiogenesis, new blood
vessels are formed by vascular endothelial cells. In fibroplasia
and granulation tissue formation, fibroblasts grow and form a
new, provisional extracellular matrix (ECM) by excreting
collagen and fibronectin. Concurrently, re epithelialization of
the epidermis occurs, in which epithelial cells proliferate and
‘crawl’ atop the wound bed, providing cover for the new tissue
(Figure 3.3).
In contraction, the wound is made smaller by the action of
myofibroblasts, which establish a grip on the wound edges and
contract themselves using a mechanism similar to that in smooth
muscle cells. When the cells’ roles are close to complete,
unneeded cells undergo apoptosis. In the maturation and
remodelling phase, collagen is remodelled and realigned along
tension lines and cells that are no longer needed are removed by
apoptosis.
Regeneration
In the regeneration phase, blood vessels are repaired and new cells
form in the damaged site, similar to the cells that were damaged
and removed. Some cells, such as neurons and muscle cells
(especially in the heart), are slow to recover. If the injury is minor
then it is possible to return the injured tissues to their original
structure and function through regeneration. However, if the
injury is severe then regeneration is not possible and repair will
not take place. Both regeneration and repair begin with phagocy-
tosis, which includes fibrin from dissolved clots, microorganisms,
erythrocytes and dead tissue.
Three phases occur in repairing the wound. These are the
migratory, proliferative and maturation phases. In the migratory
phase, the clot becomes a scab and epithelial cells migrate
beneath the scab to bridge the wound. During the proliferative
phase there is extensive growth of epithelial cells beneath the
scab, deposition of collagen fibres by fibroblasts and continued
growth of blood vessels. In the maturation phase, the scab drops
off as the epidermis returns to normal thickness. In the dermis
the, collagen fibres become more structured, fibroblasts decrease
in number and blood vessels are restored to their normal
function.