Everything from Bottles and Breathing to Healthy Speech Development
by Diane Bahr, MS, CCC-SLP, NCTMB, CIMI
Author of Oral Motor Assessment and Treatment: Ages and Stages
(Allyn & Bacon, 2001)
All marketing and publishing rights guaranteed to and reserved by:
Sensory World
www.thesensoryworld.com
721 W. Abram Street
Arlington, TX 76013
Toll-free: 800-489-0727
Phone: 817-277-0727
Fax: 817-277-2270
Web site: www.FHautism.com
E-mail: info@FHautism.com
All rights reserved.
© 2010
Printed in Canada
Cover design: TLC Graphics
Interior design: Publication Services, Inc.
No parts of this publication may be reproduced by any means without the express written permission of Sensory World.
ISBN 13: 978-1-935274-35-3
To all of the children and families with whom I have had the pleasure to work, particularly Cris, Tony, and baby Anthony, who helped me gain momentum in writing this book. A special thank-you to the lactation consultants at Greater Baltimore Medical Center (Cindy, Dee Dee, Marla, and Peg), who sent many babies my way and constantly inspired me. To my husband Joe, who provides me with continuous support and caring. And to my daughter Kim, who taught me about babies in the first place.
“Diane, you’ve got a gem here...your book is a well-organized resource that is chock full of new information and ideas in an easy-to-read format. It’s an extremely valuable book—valuable to parents who are troubled about their child’s feeding or speech difficulties and don’t know where to turn, and valuable to speech therapists who seek sensible and practical answers to apply in their own therapy. Thank you for your creation and compilation of this highly useful material!”
Char Boshart, MA, CCC-SLP, Speech Dynamics, Inc
“This book provides a wonderful resource, full of beneficial information and practical ideas to support our international community of parents. Diane shares the secrets of her expertise and experience, providing us with a guide to best practice in the areas of feeding and speech development for infants and young children. Her dedication to writing this for parents is a gift to all of us, parents and professionals alike.”
Mari Caulfield, Speech and Language Therapist, Galway, Ireland
“This much-needed book helps parents identify possible feeding and speech problems early and provides a wealth of practical advice and strategies from infancy up, to help secure the best possible prognosis for the child’s future development. It’s a treasure for anyone that cares for children.”
Lisa Geng, Coauthor of The Late Talker: What to Do If Your Child Isn’t Talking Yet and President of The Cherab Foundation
“What an informative book! Whether you are searching for everyday activities you can use to encourage your child’s feeding, speech, and mouth development, or you are interested in exploring the mechanics of these skills, this is great resource, filled with nuggets for parents and professionals.”
Dr Debra Jervay-Pendergrass, Linguist, Speech-Language Pathologist, Early Language-Literacy Consultant, and Director of the “First Stories” Project
“Diane’s book is great, and should be in every parent’s hands! There is no other reference for helping parents understand the connection between feeding, speech, and mouth development. Finally—a comprehensive, invaluable resource with the practical information parents need for one of their top parenting concerns: successful feeding!”
Nina Ayd Johanson, MS, CCC-SLP, CEIM, Feeding Specialist and Certified Educator of Infant Massage
“It has been my pleasure to work with Diane to more effectively help babies with breastfeeding difficulties. My hope is that this book will foster more teamwork among feeding professionals and give parents a better idea of how their baby’s mouth develops. Most breast-feeding problems can be prevented or corrected with better understanding and proper help.”
Peg Merrill, BS, IBCLC, International Board Certified Lactation Consultant
“If you find the introduction fascinating—wait till you read the book! Infant feeding and normal development is my specialty, so it’s nice to see a book that helps all children achieve good feeding and eating skills. The strategies to assist bottle-feeders are long overdue—since about 1975. There are still some health professionals who think that books for parents are ‘not for them’—this one will teach everyone something!”
Ailsa Rothenbury, MA, RN, CHN, IBCLC, author of Breastfeeding Is Not a Spectator Sport: Strategies for the Domestic Coaching Team
“As both parents and physicians, we were able to appreciate Diane’s work and teachings on many different levels. Her book serves as a superb educational tool to both parents and other health professionals interested in feeding. We especially feel that this book should be mandatory reading for every single pediatrician and pediatric gastroenterologist. Feeding is such a complex issue that it requires the collaboration of specialists in several different disciplines—such as speech-language pathologists, occupational therapists, dieticians/nutritionists, pediatricians, and pediatric gastroenterologists—working together to ascertain the right diagnosis to develop the proper solution and effective treatment. It is Diane’s unique insight into this often-difficult matter that brings solutions that can be implemented by parents and professionals alike to promote health and well-being to our children. We believe that Diane accomplishes this through this exquisitely written book. Congratulations, Diane, you did it!”
Inga Polyak, MD, and Mark Degen, MD, DDS
“Diane Bahr’s new book, Nobody Ever Told Me (or My Mother) That! Everything from Bottles and Breathing to Healthy Speech Development, shares all her expertise and is the gold standard for parents to easily understand and assist in their child’s development.” Susan Harrison, Parent of a child with special needs
“Full of useful, field-tested advice on your child’s feeding, speech, and oral motor development—this gem of a book reaches out to parents across cultures and boundaries.”
Christine Tan, Parent Support Coordinator, Ovspring Developmental Clinic, Singapore
“Bahr’s new book provides a wealth of information for parents. Her extensive clinical experience and personal knowledge demonstrates her insight into the needs of parents. New parents will find the charts especially helpful in preparing for visits with medical professionals. It is always difficult for a parent to remember all that they want to discuss at a medical visit. This is a resource they can write in to log developmental milestones, identify concerns, carry with them to an appointment, and use as a starting point for discussion with their pediatrician, dentist, etc.”
Pat Taylor, MEd COM, CCC/SLP
This book reflects the ideas and opinions of the author. Its purpose is to give the reader helpful information on the topics covered in the book. It is not meant to provide health, medical, or professional consultation. The reader is advised to consult appropriate health, medical, and other professionals for these processes. The author and publisher do not take responsibility for any personal or other risk, loss, or liability incurred as a direct or indirect consequence of application or use of information found in this book.
I would like to acknowledge the many extraordinary people who assisted me in the completion of this book. If I have forgotten anyone, I sincerely apologize.
First, I would like to thank Cris and Anthony Fotia for allowing me to use the photographs of their fabulous son, Anthony, Jr, in this book, and artist Anthony Fotia, Sr, who created original artwork for the book. In addition, I would like to thank the many parents and colleagues who helped to make this the best book possible.
To those who read, reviewed, and made suggestions for the entire book:
Susan Abbott, PhD, CCC-A/SLP, Assistant Professor, Stephen F. Austin State University
Daniela Rodrigues, MA, CCC-SLP, Trilingual Speech-Language Pathologist
Sara Rosenfeld-Johnson, MS, CCC-SLP, Inventor and Entrepreneur
Sheryn Wright, Master-Level English Teacher
To those who read, reviewed, and made suggestions for appropriate sections of the book:
Charlotte Boshart, MA, CCC-SLP
Chris Brown, Parent
Anthony Fotia, Parent
Dee Dee Franke, RN, BSN, IBCLC
Catherine Watson Genna, BS, IBCLC
David Hammer, MA, CCC-SLP
Kathleen A. Harrington, MA, CCC-SLP
Susan Harrison, Parent
Deborah Hayden, MA, CCC-SLP
Christina Johanson, MS, CCC-SLP
Nancy Kaufman, MS, CCC-SLP
Raymond D. Kent, PhD, CCC-SLP
Debbie Lowsky, MS, CCC-SLP
Pamela Marshalla, MA, CCC-SLP
Cindy McCartin, RN, BSN, IBCLC
Peg Merrill, BS, IBCLC, RLC
Suzanne Evans Morris, PhD, SLP
Marla Newmark, RN, BSN, IBCLC
David C. Page, DDS
Brian Palmer, DDS
Donna Ridley, MEd, CCC-SLP
Jaime Sandlin, Reader
Mary Sandlin, Parent
Will Schermerhorn, Parent
Mary Shiavoni, MS, CCC-SLP
Patricia Taylor, MEd, COM/CCC-SLP
Alicia Wopat, Parent
To Christine Tan of OvSpring Developmental Clinic in Singapore, who introduced me to David Brown, JD.
To Polly McGlew, JD, and David Brown, JD, who encouraged me to write this book and worked with its first writing.
To my outstanding editor Heather Babiar, who truly understood the information I was trying to convey and helped me to say it.
To the Gilpins of Future Horizons, my wonderful publisher, originally from my home town of Baltimore. Thank you Jennifer, Wayne, and Kelly.
To the staff at Publication Services, Inc., who made this a beautiful book.
READER’S NOTE
ACKNOWLEDGMENTS
FOREWORD
INTRODUCTION
CHAPTER 1: LET’S LEARN ABOUT YOUR NEWBORN BABY’S MOUTH
Differences between Your Mouth and Your Newborn Baby’s Mouth
Your Newborn Baby’s Mouth Reflexes
CHAPTER 2: SECRETS FOR BETTER BREAST-AND BOTTLE-FEEDING
Important Mouth Characteristics for Feeding
The Best Positioning for Feeding Your Baby and Why
What Breast-Feeding Can Do for Your Baby’s Mouth That Bottle-Feeding Cannot
Help with Nursing/Breast-Feeding
Finding an Appropriate Bottle Nipple
What to Do If Your Baby Has Difficulty Maintaining a Latch
What to Do If Liquid Is Flowing Too Fast or Too Slowly
Subtle Difficulties That Can Affect Feeding and What to Do about Them
Nutrition
Hydration
Feeding Development: One to 6 Months of Age
Feeding Development Checklist: One to 6 Months of Age
CHAPTER 3: BREATHING THROUGH THE NOSE, BELLY TIME, ALLERGIES, SPIT-UP, SIDS, AND VACCINES
The Importance of Breathing through the Nose for Health
The Importance of Belly Time When Your Baby Is Awake
Health Problems and Possible Treatments
Let’s Talk about Allergies and Sensitivities
Reflux, SIDS, and Sleeping on the Back
What about Vaccines?
CHAPTER 4: THE HAND-MOUTH CONNECTION: HELPING YOUR BABY HAVE MOUTHING EXPERIENCES THAT PROMOTE GOOD DEVELOPMENT
The Hand-Mouth Connection
The Importance of Good Mouth Experiences
Appropriate Pacifier Use and Thumb- and/or Finger-Sucking
Weaning Summary
Teething and Drooling
What to Do about Too Much Drooling
CHAPTER 5: MASSAGE, “JAWS-ERCISE,” TOOTH-GRINDING, BUBBLES, AND HORNS
Face, Jaw, and Mouth Massage with “Jaws-ercise”
Mouth Toys and More “Jaws-ercise”
What to Do about Tooth-Grinding
Horn and Bubble Play
CHAPTER 6: SECRETS FOR BETTER FEEDING BEGINNING AROUND 5–6 MONTHS OF AGE
Positioning Your Baby for Higher-Level Feeding Activities
Jaw Support
Spoon-Feeding
Drinking from a Cup
Drinking from a Straw
Taking Bites and Chewing Safe, Appropriate Foods
Introducing Foods and Liquids
How Much Do I Feed My Child?
Weaning from the Bottle and Breast
Feeding Problems and Picky Eating
Example: Emily, Aged 12 Months
Feeding Development from 5 to 24 Months of Age
CHAPTER 7: THE SECRETS TO GOOD SPEECH DEVELOPMENT
Tips to Encourage Good Vocal Development and Speech Development from Birth
Speech Sound Development from 1 Month of Age to 8 Years
Essentials for Intelligible Speech Production and Communication
Speech and Communication Development Up to 3 Years of Age
What to Do If Your Child Is Not on Track with Speech and Communication Development
A Combination of Specific Treatment Ideas for Young Children with Speech and Communication Problems
CHAPTER 8: YOUR CHILD’S BEST NATURAL APPEARANCE
What Your Child’s Face and Mouth Should Look Like
Treatments Offered by Dental and Other Professionals
Face, Mouth, and Vocal Development through Adolescence and Early Adulthood
CHAPTER 9: WORKING WITH PROFESSIONALS
Suggestions for Finding and Working with an Appropriate Professional
Your Child’s Lactation Consultant, Pediatrician, and Other Medical Professionals
Speech-Language Pathologists and Audiologists
Occupational Therapists
Other Professionals You and Your Child May Need or Encounter
Teams
CHAPTER 10: HOW DOES THIS APPLY TO MY CHILD WITH PARTICULAR SPECIAL NEEDS?
Children Born Prematurely
Children with Down Syndrome
Children with Autism
Children with Cerebral Palsy
Children with Hearing Loss
Children with Other Developmental Delay
A Few Comments Regarding Treatment of Children with Cleft Lip and Palate
APPENDIX A: RESOURCES FOR PARENTS AND CARE PROVIDERS
Articles, Books, Materials, and DVDs
Web Sites
APPENDIX B: ADDITIONAL RESOURCES FOR PROFESSIONALS
NOTES
INDEX
Awareness is the first step toward change. Through the eye of awareness, parents and professionals first gain an understanding of how a process such as the development of feeding skills unfolds. Awareness without judgment enables them to apply general knowledge and observation to specific children and make better decisions.
Infants and young children are highly resilient. Most have the internal sensory and movement abilities to adjust to feeding situations that are less than ideal. They learn to eat and drink in spite of irregular schedules, poor positioning for nursing, spoons that are too large, or food textures that are too challenging for their current experience and skills. They may struggle or protest, but eventually they learn, because taking in enough food and liquid is essential to life and survival.
Some children are born with poorer coordination, a high level of sensitivity to their environment, allergies, or structural difficulties that make eating and drinking exceptionally challenging. Some babies and toddlers, such as those born prematurely, simply need more time and adult guidance to develop these skills. When they are offered eating challenges that are too difficult or experience foods or feeding utensils that don’t fit their current needs, they may become discouraged or frustrated; some may even refuse to eat whole categories of food or reject the spoon or cup because they associate it with discomfort or failure.
This is a book that builds awareness. Diane Bahr asks the simple question, “Do children learn more easily when parents understand their needs and the significance of the various stages of development?” Her answer is a clear “yes.” Many parents worry that something is wrong with a child when their baby doesn’t do things that they remember an older brother or sister doing at the same age. They become fearful that their baby will never be able to chew or drink from a cup. If there are feeding difficulties, someone may tell them that their child will be delayed in speech development. When parents are afraid, their emotions get in the way of their ability to connect lovingly with their child. They may pull back from the relationship in their concerns about the baby’s development. Their own stress levels can make it harder for their youngster to move freely into newer skills.
This is a book about babies and young children. It is secondarily about how their mouths and faces develop for feeding and early speech. It is a book about parents and their desire to support their child’s natural development. Diane provides guidance that enables parents to understand their baby’s development of feeding and to see it in relationship to everything else that the baby is doing. It can assure them that their baby is developing in the same way as other infants, setting his own pace and timing in learning something new. It also offers parents ways to observe and understand when feeding and speech development have become stuck and their baby doesn’t seem to be moving to the next level. When feeding and speech are not progressing well, this book offers suggestions that parents can incorporate into their daily life and describes various professionals and other resources that can help them.
Suzanne Evans Morris, PhD
As a feeding and speech therapist for almost 30 years, I have seen many children with health and development concerns directly related to problems with feeding and other early mouth experiences. These include sinus and ear problems, allergies, asthma, gastroesophageal reflux, nutritional concerns, sensory processing concerns, late vocal and speech development, and orthodontic issues. Many of these problems could be avoided or reduced if parents and other caregivers had more specific information and training on these topics.
The information in this book comes from my years of experience as a speech-language pathologist while working with children on the development of improved feeding and communication skills. The book also contains the best research I could find on the topics presented. I will tell you the secrets many therapists have learned over the years that the typical parent may never hear, information your child’s pediatrician may not know to tell you. I wish I had had this information when I was a young mom more than 30 years ago.
There are many books on breast-feeding, childhood nutrition, and child development, but I have not found any book for parents that outlines the mechanics of feeding, speech, and mouth development. Good feeding techniques and appropriate mouth activities are essential for your child’s overall health, well-being, and, ultimately, proper speech development.
Today, parents often do not have the role models of extended families living nearby to demonstrate techniques that were used successfully by previous generations. This information is not innate in our modern world, and feeding can become a tedious pattern of trial and error for parents and their babies if they don’t have help.
Just ask some parents:
There are horror stories about children who refuse to eat an appropriate variety of foods necessary for basic nutrition. Many of these struggles began with incorrect and/or unsuccessful feeding techniques. Speech-language pathologists are also seeing an increase in the number of children with late-developing speech. These are often the same children who had feeding problems.
The ideas presented in this book help parents and other caregivers solve these problems easily and naturally. Giving parents the appropriate tools to feed their baby and stimulate his or her mouth development is crucial for decreasing parent anxiety and frustration, as well as increasing positive interactions between parent and baby. In his book The Happiest Baby on the Block, Dr Harvey Karp says that parents who succeed in feeding and calming their babies “feel proud, confident, and on top of the world!”1 What could be more important than proper nutrition and good communication?
By using the simple, appropriate techniques presented in this book, you will:
Just follow these simple, healthy guidelines as you go through your everyday activities with your child. They will make your life easier and eliminate the guesswork. This is a guilt-free, pressure-free, success-oriented approach, so you can have more fun and enjoy watching your child develop these marvelous new skills.
Some special features of this book include:
The book contains 10 chapters that are easy to understand and use.

Good mouth development is extremely important for the health and well-being of your baby. The mouth is not only the route to good nutrition, but it is an area through which your child will gather information about the world and ultimately learn to express him- or herself through speech.
Birth to 2 years of age is a critical learning period for mouth skills. This is the time when your child will develop the majority of his eating and drinking skills used throughout life. It is also the time when your child will begin to speak. Significant changes in your baby’s mouth structure and movement (function) occur at this time. These structure and function changes assist with the many new mouth skills your baby is learning.
Now, you might be wondering why this is important for you to know. Well, getting acquainted with your baby’s mouth from the start will help you understand feeding and other aspects of mouth development as your baby grows. If a problem does arise, you will know what to do or where to go for help. I have seen and worked with many frustrated parents whose children had small feeding and speech problems that turned into larger problems over time. My goal is for you to feel successful in your child’s feeding and speech development from the beginning.
In this chapter, you will learn the differences between the structure of your mouth and your baby’s mouth, as well as how your newborn baby’s mouth moves and works from birth. There will be two hands-on activities to guide you with your learning process. These activities will help you become acquainted and comfortable with your baby and his mouth.
All of the activities in this book are simple and easy to do, if you follow the directions. The activities take only a few minutes, and you will learn a lot about your baby’s mouth. For each activity, I ask you to date each statement as you discover characteristics of your baby’s mouth. This will help you build a record of your baby’s development. It will be fun to look at all your baby is accomplishing and to look back on this in the future. Think of it as a type of baby book.

Photo 1.1: Meet our model Anthony as a newborn.
Your baby’s mouth at birth is very different from your mouth. This is one reason why most babies can drink from the bottle or breast. Just try drinking from a bottle, and see how difficult this really is. It is very difficult for you, because you no longer have the mouth structures and functions most babies have at birth. Figure 1.1 shows the structural differences between your mouth and your newborn’s mouth. Activity 1.1 teaches you about these differences.
The directions for completing Activity 1.1 are listed below the Activity 1.1 checklist. Please follow these directions to help you understand the details of the checklist. The checklist, by itself, does not explain what you need to know.
THE MOUTH AND PHARYNX OF THE NEWBORN
(sagittal section)
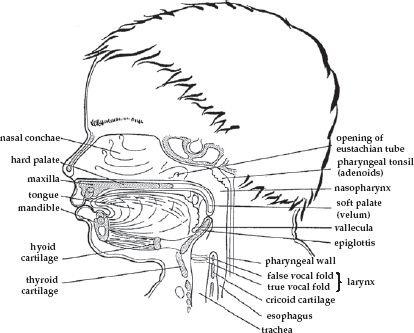
THE MOUTH AND PHARYNX OF THE ADULT
(sagittal section)

Figure 1.1: Structural differences between the newborn and the adult mouth and pharynx.
Source: Reproduced with permission of Suzanne Evans Morris. Original artwork of artist Betsy True.
You will need to trim your fingernails for the activities in this and other chapters. You may also want to use disposable gloves for these activities. You can buy these at the pharmacy or medical supply store or get them from your dentist. Ask for nonlatex, nonpowdered gloves that are made to go into the mouth. Some other gloves taste bad, smell bad, and are made of latex (a common allergen).
Now, let’s have some fun exploring your baby’s mouth. This is your newborn baby’s “window to the world.” You are going to be placing your finger into your baby’s mouth to calm him anyway, so you might want to know something about where you are going.
Important Note: If your baby is not in the mood for you to explore his mouth, wait until he is in the mood. Babies usually enjoy this. Your baby will be the leader in the process of mouth exploration. You will watch your baby’s facial expressions and body language to see if he is enjoying the process.
Some babies do not enjoy mouth play as much as others. In my work as a therapist, I discovered that many of these babies have belly problems (such as reflux) from birth, which keeps them from enjoying mouth play. This seems to occur because the babies associate the discomfort of belly problems with feeding. We will talk about reflux and other health problems in chapter 3.
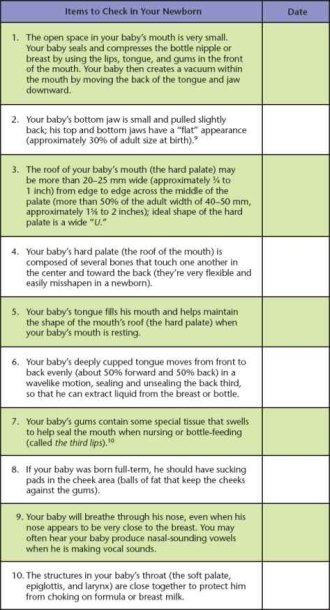
1. Look at Figure 1.1 to see the difference between your mouth and your baby’s mouth structure. Now you are ready to feel the difference. Place your freshly washed and/or gloved index finger into your newborn’s mouth (pad side down, trimmed nail side up). Feel your baby’s tongue cup around your finger. You should also feel a good suction within his mouth. This is because of the small amount of open space within your baby’s mouth.
Several mouth structures contribute to making the amount of open space within your newborn’s mouth so small. These include the size, shape, and position of the jaws and tongue, the cheek pads, and the relative position of the soft palate to the epiglottis, as seen in Figure 1.1.
The amount of open space in your newborn’s mouth is very small so that something called appropriate intraoral pressure can occur. This pressure allows liquid to be drawn into the mouth and moved back to the throat for swallowing.
Newborn babies seal and compress the bottle nipple or breast by using the lips, tongue, and gums in the front of the mouth. They create a vacuum within the mouth by moving the back of the tongue downward.11 Babies who do not have this pressure in the mouth struggle with feeding. The details of this process are discussed thoroughly in chapter 2.
2. Look at your newborn’s jaw as he is lying on his back. See how his small bottom jaw is pulled back just a little. This is typical at birth but will begin to change significantly within the first 6 months of your baby’s life. Also, if you look at where your baby’s lips meet, they will form a fairly straight left-to-right horizontal line. This reflects the normal “flatness” of your baby’s jaw. At birth, your baby’s jaw is approximately 30% of its adult size.
3. When your baby yawns or cries, take a look at the roof of his mouth. It may be a little more than 20 to 25 millimeters across the center from left to right near the middle of the mouth. Of course, you are only going to look at this visually—don’t try to actually measure it! However, you can look at a ruler to see what 20 to 25 millimeters looks like. It is approximately ¾ to 1 inch. Also, the shape of your baby’s hard palate (the roof of the mouth) should look like a wide “U.” Any other shape may indicate a problem.
4. Your baby’s hard palate (the roof of the mouth) is composed of several bones that touch one another in the center and toward the back. These bones also touch other bones that create the nasal areas, sinuses, and other parts of the skull. They are very flexible and easily moved out of position in newborns. This entire mouth roof will seem to “harden” as your baby grows.
When your baby has a closed mouth at rest (that is, when the mouth is not in use), the tongue fills the mouth to help maintain the relatively broad shape of the roof of the mouth or hard palate. The mother’s breast during nursing can also help with this process. During proper nursing, the breast is drawn deeply into the child’s mouth to help keep the shape of the palate. We will discuss mouth development in detail in chapter 8.
If you touch your baby’s hard palate, you must touch it very gently. Touching the roof of your baby’s mouth can facilitate suckling. This is probably the reason that lactation consultants often teach parents to allow the infant to suckle on the index finger (pad side up, trimmed nail side down). I teach you to turn your finger in the opposite direction (pad side down, trimmed nail side up) when you place it into your baby’s mouth for suckling if possible. This will help you avoid placing too much pressure on your baby’s very flexible hard palate.
So, why is it important for your child’s hard palate or roof of the mouth to remain fairly broad? A high, narrow hard palate will change the shape of the nasal and sinus areas. If this occurs, your child’s nasal areas and sinuses may become misshapen, and structures within the sinuses (such as turbinates) may actually block the sinuses.12
Children with small or misshapen nasal and sinus areas tend to have more sinus problems. For example, small sinuses are more difficult to clear than typically sized sinuses if your child should develop a cold or upper respiratory infection. This may lead to sinus infection and can contribute to allergies and other upper respiratory illness. Your baby may also have more difficulty breathing through the nose if the nasal and sinus areas are small or misshapen. Nose breathing is important for good health, as it ensures better development of the facial and jaw bones and directs air to the lower lung areas, where more blood is oxygenated.13 Your baby’s brain and body need oxygen for all aspects of life.
5. Look at your baby’s mouth at rest (when he is just relaxing or sleeping, not eating or making vocal sounds). Is your baby’s mouth closed? If it is, then your baby’s tongue is probably resting against the roof of his mouth. Remember, we want this rest position to help keep the shape of the palate. If your baby’s mouth is open at rest, there are some techniques in chapter 5 that can help.
6. Again, place your washed and/or gloved index finger into your baby’s mouth (pad side down, trimmed nail side up). Focus on your baby’s deeply cupped/grooved tongue around your finger. Can you feel your baby’s tongue moving front to back evenly in a wavelike motion (about 50% front and 50% back)? You may also feel the back of your baby’s tongue moving up and down at the same time (sealing and unsealing the back third of the tongue), creating a vacuum to extract liquid from the breast or bottle. Isn’t this amazing?
If you feel any differences in your baby’s mouth (such as the tongue humping—pushing up the middle of the tongue—instead of grooving/cupping, or too much or too little forward movement of the tongue), this will affect the way your baby feeds. These are subtle problems that we frequently see in babies’ mouths.
7. You may notice some enlargement of your baby’s gums when your finger is placed into your baby’s mouth. If you can’t feel this, don’t worry about it. The slight swelling of the gums that you see or feel helps your baby to seal and compress the bottle nipple or breast when drinking. These are called the third lips and will no longer be needed or seen between 3 and 6 months of age.
8. To feel your baby’s sucking pads, place the pad of your index finger inside your baby’s cheek and your thumb on the outside. Now, move your thumb and index finger up and down, front and back. You can apply some very gentle pressure between your thumb and index finger, but don’t pinch your baby. You should feel a ball of fat within each cheek. The fat pads may actually make it a little difficult for you to move your index finger inside your baby’s mouth. If you don’t feel these fat pads, the following may be true:
a. Your baby may have been born prematurely. Preemies are not born with sucking pads.
b. Your baby may have been induced or born a little early. Sucking pads develop toward the end of pregnancy, when the rest of the fat is developing on the body.
c. Your baby may have inherited thin sucking pads.
The presence or absence of sucking pads can make a significant difference in how your baby feeds. As mentioned above, your baby’s sucking pads develop toward the end of pregnancy, when the other fat is developing within the body. This is the reason that preemies are born without sucking pads.
I have worked with many babies with feeding problems who were born close to full-term and did not have adequately developed sucking pads. I often asked the lactation consultants who made the referrals why this might be. One hypothesis was that many babies are induced and may not truly be full-term. An article that appeared in The Washington Post on May 20, 2006, stated that 350,000 babies are born “slightly early” (ie, near term) in the United States each year (the average pregnancy is shortened to 39 weeks).14 Many of these children have been reported to have feeding and other developmental difficulties.
If your baby was born early (either prematurely or even a little early), your baby may not have developed adequate sucking pads. This will affect the way your baby drinks. Sucking pads help to close the mouth space by bringing the cheek areas against the gums, so that your baby has appropriate pressure within the mouth to draw in and swallow liquid.
No matter the cause, there are a number of things you can do to help your baby compensate for thin or nonexistent sucking pads. We will discuss this in detail in chapter 2.
9. Watch how your baby coordinates suckling, swallowing, and breathing. While the breast or bottle is within his mouth, he is still breathing through his nose. If your baby is breast-feeding, his nose will be very close to your breast. When your baby takes a break from feeding and vocalizes, you may hear vowel-like nasal sounds (often a short “a,” as in the word “at,” or a long “e,” as in the word “eat,” depending on whether your baby’s jaw is open or closed). The sound may be coming through your baby’s nose instead of his mouth. This will change as your baby grows. See chapter 7 for more details on speech sound development.
10. Look again at Figure 1.1, so you can see the structures in your baby’s mouth and throat. Notice that the proximity of the structures helps to make the open space within your baby’s mouth and throat very small. This helps to naturally protect your baby from choking.
Note: If you are concerned about your baby’s mouth structures or functions, talk to your pediatrician. He can refer you to specially trained therapists (eg, feeding therapists) or other professionals who can help you and your baby with these problems.
Now, let’s see how your baby’s mouth moves at birth. Your baby is born with a number of reflexes that assist with feeding until he is mature enough to make these movements on his own. These are listed in Activity 1.2.
Date each reflex as you see it in your newborn. If your baby is a little older, you can still see many of these reflexes. Your baby will not develop control over many of the reflexes for a little while. Reflexes don’t really disappear. The motor (or movement) area of your baby’s brain actually takes control over time, and your baby no longer needs the reflex to do the activity. So when you see the reflex disappearing, it means that your baby’s brain is developing.
It is fun to explore your baby’s mouth and see these in action. The directions for completing Activity 1.2 are listed below the chart. Don’t forget to trim your fingernails and perhaps wear gloves (nonlatex, nonpowdered gloves meant to be used in the mouth).
Note: If you do not see some of these reflexes in your baby’s mouth, ask your pediatrician to check for them. Also, if your baby has reflexes beyond the age when they normally seem to disappear, talk to your pediatrician. Reflexes that remain can indicate a problem with development.
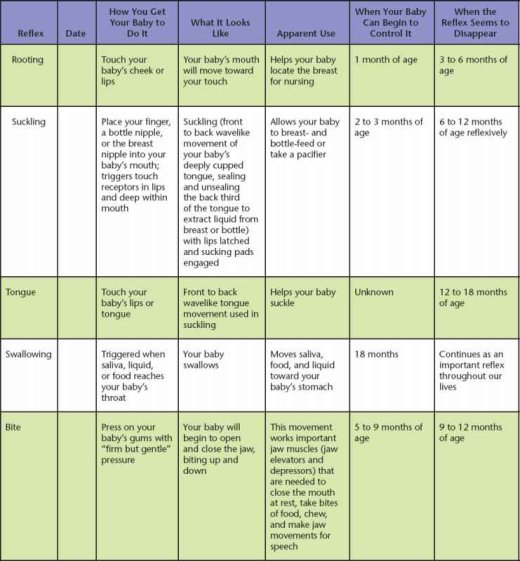
This reflex helps your baby to suckle liquids from the bottle or breast. It is stimulated by touch receptors in the lips and deep within the mouth. This is why it is important for the mother’s breast to be drawn deeply into the infant’s mouth. It is also the reason that some nurses, physicians, and therapists give babies longer bottle nipples rather than shorter ones. We will discuss the problems associated with bottle nipples that are “too long” in chapter 2.
Your baby will have the easiest time learning to suckle around the time of birth.23 This is the reason that babies should be put to the breast or given the bottle as soon as possible after birth. Your baby will begin to gain some control over this reflex by about 2 to 3 months of age. Between 6 and 12 months of age, you will no longer see your baby suckling reflexively. Twelve months of age is also the time when the mature swallowing pattern (tongue-tip touching the ridge behind the top front teeth to begin the swallow) becomes apparent. We will discuss this in chapter 6.
The bite reflex can sometimes be a problem for nursing moms. It is not a very good feeling when a baby clamps down on Mom’s breast. This can usually be avoided if your baby is breast-feeding properly. See chapter 2 for further details. Babies develop control of the bite reflex between 5 and 9 months of age, when they are learning to take bites and chew foods. The reflex seems to disappear between 9 and 12 months of age, when chewing and taking bites of food are well established.
Through feeding and other important mouth experiences, your baby’s gag reflex will eventually move to the back quarter of the tongue. This is a vital process as your baby learns to handle different food textures within the mouth and goes through the critical period of discriminative mouthing. We will talk about discriminative mouthing in chapter 4.
Note: If you are concerned about your baby’s mouth structures or functions, talk to your pediatrician. He can refer you to specially trained therapists (such as feeding therapists) or other professionals who can help you and your baby with these problems.
Now that you are acquainted with your baby’s mouth, let’s go to chapter 2 and learn about breast- and bottle-feeding. Successfully feeding your baby is important for both you and your baby. Of course you know that your baby needs good nutrition to grow properly. However, in his book The Happiest Baby on the Block, Dr Harvey Karp also says that parents who succeed in feeding and calming their babies “feel proud, confident, and on top of the world!”25
Parents often receive very little instruction on ways to feed their children, yet good eating and drinking skills encourage the best mouth development. You are going to feed your child, so why not use appropriate feeding techniques that can support your child’s mouth development?
Most of our eating and drinking skills are developed in the first 2 years of life. Every 3 months from birth, your baby will have a growth spurt in this area. You can help with this process by using appropriate feeding techniques from birth.
In this chapter, we are going to address many topics related to nursing and bottle-feeding. You will learn proper breast- and bottle-feeding techniques, as well as what to do if you have a problem with either process. While I prefer that a mom breast-feed when possible, this is not always possible for some families. Therefore, we will also cover the best bottle-feeding practices.
Feeding is like dancing. You and your baby are partners in this dance. The best feeding method for you and your baby may be somewhat different from what someone else may do. As in ballroom dancing, many of the steps are similar, with specific variations that suit you and your child. However, there are some important guidelines that can help you learn the “feeding dance” easily and successfully.

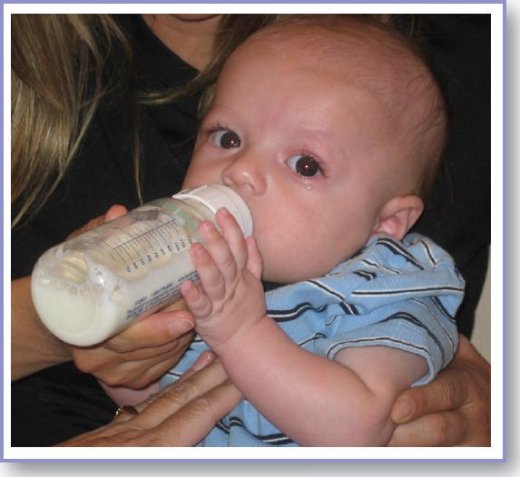
Photo 2.1: Anthony bottle-feeding at 4 months.
In chapter 1, you became familiar with your newborn baby’s mouth. Now, we are going to see how your baby accomplishes breast- or bottle-feeding successfully. Ideally, your baby should demonstrate the following characteristics, whether you are nursing or bottle-feeding. Most full-term babies are born with the potential for these characteristics. Premature and near-term babies can be assisted in developing most of them.
We will discuss these characteristics in detail. Each characteristic has been placed into bold italics, so you can locate topics easily.
Small jaw movement should occur once your baby is latched onto the breast or bottle. The tongue, sucking pads, and roof of the mouth create the right space for liquid to move safely, easily, and efficiently through the mouth. Therefore, the jaw doesn’t need to move very much.
Your baby’s tongue needs to cup or groove around the bottle or breast nipple and move 50% front to 50% back in a wavelike motion with each suckle. At the same time, the back of your baby’s tongue moves downward to create a vacuum within the mouth. This will pump the liquid from the breast or bottle easily. Babies who move their tongues too far front (sometimes called a tongue thrust or exaggerated tongue protrusion) are working too hard.
Tongue humping (pushing up the middle of the tongue) means that something has gone wrong. Children who hump their tongues and pump the liquid are working too hard and fatigue easily. They usually hump their tongues because they do not have adequate sucking pads, the tongue is tied, and/or their heads and necks are extended back. Tongue humping is an attempt to make the space inside the mouth smaller, which then adjusts the suckling pressure. This is not an efficient method for pressure adjustment within the mouth.
As mentioned previously, your baby should have even, front-to-back wavelike tongue movement.chapter 8