
in
Early Orthodontic
Treatment
Antonio Patti, MD, DUO
Director
The International Center for the Study of Clinical Orthodontics
Verona, Italy
Guy Perrier D’Arc, DDS, PhD, DUO
Former Head
Department of Orthodontics
University of Nice
Nice, France
English Translation by
Jay K. Weiss, DMD
Former Adjunct Associate Professor
Department of Human Behavior
Columbia Dental School
New York, NY


Paris, Chicago, Berlin, Tokyo, London, Milan, Barcelona, Istanbul, São Paulo, New Delhi, Moscow, Prague, and Warsaw
First published in French in 2003 by Quintessence International, Paris Les Traitements Orthodontiques Précoces
© 2005 Quintessence International
Quintessence International
11 bis, Rue d’Aguesseau
75008 Paris
France
All rights reserved. This book or any part thereof may not be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, or otherwise, without prior written permission of the publisher.
Design: STDI, Lassay-les-Châteaux
Printing and binding: EMD S.A.S., Lassay-les-Châteaux
Printed in France
To Michel and Maria Patti, my parents;
to our families; and
to our friends, C. and Y. Duchateaux, M. Cardonnet,
R. Chatagnon, and P. Vion
To Robert M. Ricketts, the father of “bioprogressive orthodontics,”
and to Carl Gugino
Acknowledgments
The authors extend their warm thanks to:
P. Collard, E. Duchateaux, T. and M. Gozzi ByArt, and G. Negriolli for their assistance in the production of the illustrations
M. Luciani, orthodontic technician, Orthoplanet Laboratory, Verona, Italy
M. Balland, for his help in preparing the manuscript
Table of Contents
| Cover | |
| Table of Contents | |
| Preface | |
| Why and When to Begin Early Orthodontic Treatment | |
| 1 | Normal Growth |
| Elements of Growth | |
| 2 | Establishment of Occlusion |
| Normal and Pathologic Development of Occlusion in Primary and Mixed Dentitions | |
| Classification of Anomalies in the Sagittal Plane | |
| 3 | Obstacles to the Development of Dentofacial Harmony |
| Mechanical Interferences | |
| Functional Interferences | |
| 4 | Diagnostic Examinations |
| Clinical Assessment | |
| Casts | |
| Photographs | |
| Radiographs | |
| 5 | Treatment of Malocclusions |
| The Concept of Unlocking | |
| Class I Discrepancies and Anomalies Common to All Classes of Malocclusion | |
| Class II Malocclusions | |
| Class III Malocclusions | |
| 6 | Appliances |
| Expansion Appliances | |
| Space Maintainers | |
| Lip Bumper | |
| Removable Appliances for Distalizing Molars | |
| Functional Appliances | |
| Posteroanterior Orthopedic Force | |
| Full-Banded Appliances | |
| Bibliography |
Preface
Why and When to Begin Early
Orthodontic Treatment
Orthodontists have made remarkable progress in their understanding of physiology, growth, tissue response, increasingly sophisticated diagnostic techniques, available materials, and information; nevertheless, with all these advances, many practitioners still find themselves at a total loss when confronted with that eternal dilemma: to intervene or not to intervene before the eruption of the complete permanent dentition.
Two opposing schools of thought exist. One philosophy is embraced by those who do not initiate treatment until the second molars and all the premolars have erupted. These clinicians assert that it is easier to begin treatment when major growth has been completed and when a treatment time of 2 to 3 years can be predicted with reasonable assurance, thereby avoiding the need to compensate for unexpected variations in the growth pattern. Often, treatment undertaken in this time framework is accompanied by therapeutic extractions and requires the use of cumbersome, complex appliances that can pose serious risks to the health of the teeth and the surrounding tissues.
Adherents of the bioprogressive school of Ricketts, Gugino, Bench, Duchateaux, Philippe, Langlade, and many others, including Fränkel, Graber, and McNamara, insist that there are many disadvantages to waiting for the 12-year molars to erupt. Not the least of these drawbacks is the failure to take advantage of the potential to eliminate or modify deviations in skeletal growth and the functional matrix (associated with mouth breathing, atypical swallowing, and other abnormal behavior) and the opportunity to orchestrate dentoalveolar development.
Beginning orthodontic treatment early seems eminently logical because it enables the complete or partial correction of many incipient discrepancies or, at least, a reduction in their capacity to grow worse. Interception—or early intervention—employs simple therapeutic techniques that do not overtax the limited stores of cooperation young patients can bring to the therapeutic encounter. Its objective is eliminating or minimizing dentoalveolar and skeletal disorders that interfere with growth, function, esthetics, and the psychological well-being of children.
“The earlier treatment begins, the more the face will adapt to your standards; the later treatment begins, the more your standards will have to adapt to the face.”—C. Gugino
Orthodontic treatment should be in harmony with modern medical thought: It is better to prevent than to cure. We should not treat the symptom; we should treat the cause. The therapeutic devices available for this endeavor are not complex, but deciding which ones to use and when to employ them is far from simple. The therapeutic choice is nothing more than the last act in a complete diagnostic process. To be capable of determining the optimum moment to begin treatment, orthodontists must possess a profound comprehension of fundamental information that forms the basis of understanding the pathogenesis of different malocclusions: normal and pathologic craniofacial growth, orofacial functional behavior, morphogenesis of the dental arches, and child psychology. Armed with this knowledge, orthodontists can accurately discern which discrepancies would benefit from early treatment and not fall into the trap of indiscriminately treating every patient they examine during the mixed dentition stage.
It is important that orthodontists perform this “triage” so that they will not get caught up in a relentless therapeutic cycle leading only to long, drawn-out treatments, patient and parent fatigue, and professional frustration. The ideal age for an initial orthodontic visit, in the authors’ view, is when the patient is about 5 or 6 years old. The goals of this first examination are to discover any discrepancies that would worsen in time; any transversal, vertical, or sagittal interferences that are disrupting normal growth; and any functional matrixes that are disturbed by mouth breathing, atypical swallowing, and postural problems, as well as destructive habits such as thumb and lip sucking.
There are three types of treatment that can be adapted to meet the clinical needs of each patient:
1. Modification of functional behavior, without appliances, through myofunctional therapy or occlusal equilibration
2. Orthopedic treatment of the maxilla or mandible
3. Treatment with simple removable or fixed orthodontic appliances
These treatments will be followed eventually by retention and reevaluation after eruption of the permanent dentition is completed: Has the intervention completely resolved the problem, or will a second phase of treatment be needed to finish aligning the teeth? The objective of early treatment is to avoid or to simplify treatment of the permanent dentition.
This volume addresses the different anomalies according to their Angle classification and with regard to their stage of development in either the primary or mixed dentition. The text has been carefully kept as concise as possible to leave adequate space for photographic documentation of clinical situations.
| Normal Growth |  |
Elements of Growth
We shall give our principal attention to the skeleton, which has been the object of the bulk of craniofacial research and is relatively easy to measure. There is no doubt that the enveloping soft tissues exert important influences on the skeleton, but these are difficult to measure directly. The methods available for studying growth utilize animals (dyed slides of tissue; evaluation of hormonal, hereditary, and dietary factors; and surgery) and humans (embryologic, genetic, and, especially, cephalometric studies).
Two types of growth
Some bones of the cranium and the face are of cartilaginous, or endochondral, origin. Others begin as membranes and are thus formed by different types of calcification, a distinction that persists only until the end of the growth period. It is important to differentiate between these two types of growth because endochondral growth is regulated, in large part, by hereditary factors, while membranous growth responds readily to forces emanating from the surrounding environment, although its prefunctional form is guided by genetic determinants. The cranial base, which develops from the primary activity of its oriented sutures, is a good example of endochondral bone growth. The bones of the cranial cap, in contrast, are membranous in origin. They are also separated by sutures, but these sutures function only secondarily to fill in the spaces that arise as growth proceeds and the developing cranial bones are propelled outward by the developing cerebrum.
Controlling factors
Growth is controlled by general and local factors. General factors include genetic, hormonal, neural, nutritional, health, and socioeconomic influences. Local factors include cartilaginous, osseous, muscular, and aponeurotic structures and functional forces.
Cranium
Here discussion will be limited to the growth of the cranial base, which is the point of support for the whole face. The cranial base consists of the horizontal portion of the frontal bone, the crista galli apophysis of the cribriform plate of the ethmoid bone, the sphenoid bone, the petrous segments of the temporal bone, and the body and the lateral masses of the occipital bone. These osseous segments are separated by synchondroses, which are active growth centers. Their orientation can be transverse or longitudinal so that they can grow in both length and width. Because it is placed obliquely, the spheno-occipital suture also allows growth in height. Surface bone remodeling can occur through apposition and resorption of osseous tissue as well as through the action of the synchondroses.
The angulation of the cranial base can influence the position of the maxilla and the mandible. This is what Björk (1963) has called “anterior rotation” or “posterior rotation” of the face. No therapeutic efforts can affect the growth of the cranial base because its outcome depends, essentially, on hereditary factors.
Middle third of the face
The bones of the face develop in two ways: by sutural growth and by remodeling.
The sutural system that unites the various osseous units of the face with each other and with the cranial base is fairly complex. These sutures are syndesmoses, which unite primarily bones that are membranous in origin. They have no inherent growth potential but, as is the case at the cranial cap, they behave like “automatic joints of expansion and shrinkage that operate through adaptive connective tissue proliferation and marginal calcification” (Delaire 1971, 1978). These are the “functional units” that Moss (1982) asserts have the primary responsibility for the movement and development of the osseous segments. Making these phenomena complex are the great number of syndesmoses, the variation in their orientations, the variation in the timing and extent of their activity, and the rapid decrease in the intensity of their action as growth proceeds.
Remodeling, which becomes more important as sutural activity declines, is expressed as surface apposition in some regions and resorption in others. It leads to morphologic changes, which include the development of the sinuses.
Mandible
The mandible is primarily a membranous bone that forms around Meckel’s cartilage, which, after serving as a guide for development, disappears. The growth of the mandible takes place partly in response to the activity of condylar cartilage and partly through recontouring.
Alveolar processes
The alveoli have traditionally been considered to be osseous tissue that is created when the teeth appear and disappears when they are lost.
The dental arches develop by heavy apposition of bone, tied to the development of the dentition. The arches diverge posteriorly, thus increasing their volume enough to accommodate the erupting molar teeth.
The growth of the alveolar processes contributes significantly to facial height. Once established, the transverse dimensions of the arches are more or less constant. The distance between the canines becomes fixed between the ages of 8 and 10 years.
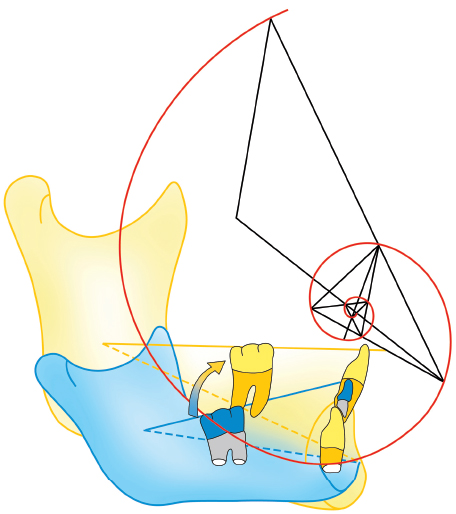
The dentoalveolar arches respond to stimuli from the musculature and from other surrounding centrifugal and centripetal functional forces generated by the tongue, lips, and cheeks; from the extrusive action of erupting teeth; and from the intrusive action of the muscles of mastication that model and shape them by forming what Chateau (1993a) calls the dental corridor and Gugino (2000) refers to as the neutral zone (Fig 1-1).
Facial type
To study the malformations that afflict young people, orthodontists must understand facial types so that they can predict the way a face will evolve, formulate a treatment plan, and establish a prognosis. Apparently similar malocclusions should be treated differently in patients whose typology is dissimilar.
Björk (1963) has described facial typography in detail. According to him, the maxilla should move downward and forward away from the cranial base, making an angle of 51 degrees with the sella turcica–nasion line (Fig 1-2). In fact, this angle can range from 0 to 82 degrees, which means that, during the period observed (5 years 8 months to 13 years 8 months), the displacement can be entirely horizontal or virtually vertical with respect to the cranial base. The average value is only relative; individual variations, which are frequent, must be taken into account.

Fig 1-1 The dental corridor, or neutral zone.

Fig 1-2 During growth, the maxilla moves downward and forward away from the cranial base, according to Björk (1963).
For the mandible, Björk’s classic description (1963) posits two opposite typologies that he called anterior mandibular rotation and posterior mandibular rotation (Fig 1-3). These variations arise from differing patterns in the vertical growth zones, which are the maxilla and the posterior segments of the mandibular and the maxillary alveolar processes.
Condylar growth alone propels menton forward. When this impetus joins with vertical alveolar growth, menton tends to move backward and forward.
When the two growth zones do not operate in harmony, the mandible rotates. Growth is normally most active in the region of the alveolar processes. If growth of the condyle outpaces that of the posterior alveolar process, the mandible rotates counterclockwise; as a result, menton advances, an incisal overbite might develop, and lower facial height will be diminished. On the other hand, if alveolar growth is greater than condylar growth, the mandible will rotate clockwise. Menton will move downward and backward, and lower facial height will increase.
Molar height not only influences the vertical position of menton but also to a great extent controls, by its anteroposterior position, the degree of mandibular rotation. This explains why vertical anomalies are often responsible for anteroposterior discrepancies and why, clinically, the orthodontist should be careful to monitor and control the vertical dimension during treatment.
By analyzing cephalometric radiographs, the orthodontist can determine a patient’s facial type (see chapter 4 on cephalometrics). Ricketts (1961) described a brachyfacial type that corresponds to anterior mandibular rotation, a dolichofacial type that corresponds to posterior mandibular rotation, and a mesofacial type that corresponds to the average type.

Fig 1-3 The two types of mandibular growth and their characteristics, according to Björk (1963).
Fig 1-3a Anterior mandibular rotation: (1) condylar head oriented high and forward; (2) mandibular canal with exaggerated curvature; (3) closed mandibular angle; (4) inferior border of mandible without pregonial notch; (5) symphyseal axis oriented upward and forward (axis of mandibular incisors not in harmony with symphyseal axis); (6) thick subcortical plate; (7) open posterior interdental angles; (8) diminished lower facial height.
Fig 1-3b Posterior mandibular rotation: (1) condylar head oriented high and backward; (2) mandibular canal with mild curvature; (3) open mandibular angle; (4) condylar border of mandible with pregonial notch; (5) symphyseal axis inclined upward and backward (axis of mandibular incisors in harmony with symphyseal axis); (6) thin subcortical plate; (7) closed posterior interdental angles; (8) increased lower facial height.
Rate and rhythm
When orthodontists treat young children, these patients will be going through periods of rapid growth that will often make greater overall contributions to changes in facial appearance than the treatment itself. The orthodontist must determine not only the patient’s facial type but also the direction, rate, and amount of facial growth. The orthodontist can also obtain useful information by evaluating statural growth, because the face in general, the maxilla, and especially the mandible grow at the same rate as the body as a whole.
The maxilla stops growing before statural growth terminates, but the mandible continues to increase in size even after full stature has been reached (Björk 1963).
After the completion of statural growth, the remaining growth of the mandible is not negligible.
The orthodontist should know each patient’s level of development according to the growth curve. The clinician can verify a patient’s stage of maturation by assessing three criteria:
1. The observed rate of statural growth
2. The stage of calcification
3. The degree of sexual maturation
To determine the optimum time to begin dental orthopedic treatment, the orthodontist should know the patient’s growth rate and rhythm, which can be difficult to estimate because of the great individual variations among patients. The orthodontist can utilize some specialized techniques to determine the period of maximum growth before the prepubertal peak and to locate the individual patient’s stage of development on the growth curve (Fig 1-4). One method is to take radiographs of the wrist and compare them to standardized tables that indicate the stage of bone maturation or “osseous age.” This method, however, gives only an approximate reading.
Optimum time to begin treatment
By judiciously planning the full range of the proposed dentofacial orthopedic and orthodontic therapy in harmony with the chronologic age, the degree of osseous maturation, and the dental status of their patients, orthodontists can avoid drawing out treatments into that perilous region where both children and parents grow weary, dissatisfied, and uncooperative.

Fig 1-4 Growth curve (Björk 1963). Skeletal growth can be divided into five stages. It is rapid from birth until about 30 months (early infancy). Björk does not include this stage in his growth curve. The rate of growth thereafter diminishes swiftly, reaching a low point at around 6 years (infancy or middle infancy period). This is the time when preventive orthodontic measures can appropriately be taken. Growth remains relatively stationary until the prepubertal period is reached at 10 to 11 years of age in girls and 12 to 13 years in boys. This late infancy, or juvenile, period is the stage during which orthodontists can undertake interceptive procedures. The prepubertal or pubertal growth spurt follows, from 10 or 11 years to 15 or 16 years in girls and from 12 or 13 years to 18 years in boys. This is the most appropriate stage for the initiation of orthodontic or dentofacial orthopedic treatment. From then on, growth diminishes progressively, terminating at 15 to 17 years in girls and at 18 to 20 years in boys, when the period of youth is considered to be at an end. From an orthodontic point of view, there is no further growth in this adult stage; any planned treatment will have to be compensatory or surgical.
| Establishment of Occlusion |
 |

Normal and Pathologic Development of Occlusion in Primary and Mixed Dentitions
The morphogenesis of the dental arches occurs discontinuously, alternating between active and stable phases, and proceeds for about 20 years.
Eruption schedule of the primary dentition
The timing of eruption is highly variable, so these values are only approximate:
1. At 6 months: primary mandibular incisor
2. Between 6 and 13 months: the other primary incisors